The inequalities that Canadian female employees facing in health care occupations
Overview
The three typical types of inequalities towards female employees are less female in leadership positions, workplace abuse and sexual harassment towards female health care industry workers, and gender-stereotyping comments towards female employees. Until 2020, female constitute 82% of health care workers in Canada, in contrast to 47% in the total labor force[1] . This rate goes over the international rate of 75%. During the past 9 years, the health occupation staffs increased approximately 69%, almost twice that of the Canadian labor force[1] . The proportion of female in health care industry has a faster growing rate than male, which is 72% female employee versus 55% male employees[1].
The roles in health care industry relevant to gender stereotype include:medical assistant, nurse assistant, licensed practical nurse, physician, therapist[2], etc.
Less female in leadership positions
Although there are 82% of Canadian female works in health care industry, female Health care workers' participation in leadership position is almost invisible[1] . This happens to remain underrepresented in leadership positions, also not only at the highest levels of management[3]. There is a glass ceiling in health care occupations towards female, similar to other occupations. Only 30% of Canadian female health care workers are in leadership positions in hospitals and other health care organizations, while the other 70% leaderships positions are occupied by males. In Ontario, as of 2018, there are only 5 female CEOs among the 23 academic hospitals[1] .
The inequality of female leadership in health care industry is caused by both “cultural assumptions about women leadership capability to systemic gender barriers[1] . It means the policies, practices or procedures result in some people receiving unequal access or excluded. It is usually referred to as a “glass ceiling” because it prevents female from advancing to management positions[1] ”
Workplace abuse and sexual harassment
Surveys of Canadian nurses show that: About 1/3 to 1/2 of nurses have experienced physical abuse. In addition, approximately 3/4 of them have reported verbal abuse which usually includes discriminatory language, sexually harassing language, and inflammatory behaviour by coworkers or bosses[4]
The research indicated “female in health care occupation are more likely to experience sexual harassment at work when they are seen as subservient or are isolated from other co-workers, such as live-in domestic caregivers, health care worker, and massage therapists[5]” Also, O'Connell & Korabik’s research indicated male patients and male colleagues are more likely to abuse female workers, since they have more opportunities to interact with potential targets[6] .
The report of Canadian Federation of Nurses Unions indicated the violence towards Canadian female health care workers are caused by “under-staffing, inadequate security and increased patient numbers" [4].
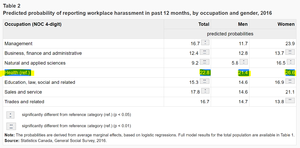
Statistic
According to Statistic Canada, workers in Health occupation are the most likely to report having been harassed on the job in the past year at 23% because the gender distribution of health care occupations.[7].
Source: https://www150.statcan.gc.ca/n1/pub/75-006-x/2018001/article/54982-eng.htm
Facts about work place abuse and harassment
“Difficult to return to work because of low self-confident” is one of the most important consequences of workplace abuse[8]. The economic related factors adding more difficulties for employees to report about the improper and seek help. Even female employees in positions of authority experienced sexual harassment or inappropriate gender-related behavior[4]. Work place abuse also has a critical influence toward Canadian economy because the work place abuse led to physical and psychological problems in abused victims. This reduced workplace productivity by 0.5 billion per year [9] The other economic facts towards discrimination is, not like factors of years of education or work experience, "gender" is the an unadjusted factor that affect female in health care occupations. [10]
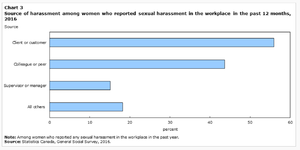
The type of perpetrators
Source:https://www150.statcan.gc.ca/n1/pub/75-006-x/2018001/article/54982-eng.htm
The perpetrators of sexual harassment in health care industry includes clients or customer, colleague or peer, supervisors or manager, and others.[7]
#MeToo Medicine campaign
As a movement against sexual assault and sexual harassment, the #MeToo campaign was created by Tarana Burke, a social activist that began using this phrase since 2006. In October of 2017, the #MeToo campaign went viral as actress Alyssa Milano tweeted about it [11] .The #MeTooMedicine campaign has brought attention to the female employees in health care industry that have been quiet for a long time. It became a place that females health care employees bravely share the experiences of sexual harassment and work discrimination. The covered range is from sale representatives to top management staffs[12] .
Gender-stereotyping comments towards female employees
“Nurse, can you get me another blanket?” “I’m a doctor. I wonder why many people make that mistake.”[13]. This conversation is not surprise that female physicians are frequently mistaken for nurses or other health care specialists. [c] The gender-stereotyping assumption that all medical doctors are male has underestimated the competency of female physicians. The consequence is that female doctors are frequently being called as nurses or sweeties. Moreover, this gives the assumption that female doctors are inexperienced and incompetence, so patients often ask intrusive personal questions and doubt their medical capacities.[13] One reason that people assume female doctors as nurses is because people believe females are better at nurturing, since it is an extension of their domestic roles. The stereotyped image of nurse usually have characteristics of subordinate, nurturing, domestic, humble, self sacrificing as well as not too educated became prevalent in society." [14]
In reality, female doctors are better at treating their patients because they allocate more time and are attentive to patients' medical and psychological needs. The research indicated “compared with male physicians, women spend more time with their patients, offer more follow-up care, more likely to address mental health concerns and establish collaborative partnerships with their patients[15] ". However, in Canada, most physicians are paid by the government according to how many patients they see in specific amount of time. This arrangement explains the reason female doctor earn 26% lower than male doctor, since they spend longer time with each patient, and they need balance the career with family in different ways than their male counterparts.[15]
Negative impacts
The gender inequality and discrimination negatively affect female employees in health care industry by low career satisfaction, negative effect to employee’s mental as well as physical health, and unequal compensation. Obviously, the current government policy is not adequate enough for protecting female health care worker’s right. In order to eliminate the discrimination towards Canadian female in health care occupation, aligning with the Canada’s G7 Presidency, a fundamental shift of promoting gender equality towards the female employee’s is critical[16].
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Tang, Justin (April 2018). "Women's work across every aspect of healthcare is largely invisible". making evidence matter.
- ↑ Top Medical Assistant Schools (2020). "Top 50 Health Care Jobs". Top Medical Assistant Schools.
- ↑ Berlin, Gretchen (June 7, 2019). "Women in the healthcare industry".
- ↑ Jump up to: 4.0 4.1 4.2 The Canadian Federation of Nurses Unions (2017). ENOUGH IS ENOUGH, PUTTING A STOP TO VIOLENCE IN THE HEALTH CARE SECTOR. Ottawa, ON: The Canadian Federation of Nurses Unions. ISBN 978-0-9868382-9-3.
- ↑ "Sexual harassment & sex discrimination at work". 2019.
|first=missing|last=(help) - ↑ "Sexual Harassment: The Relationship of Personal Vulnerability, Work Context, Perpetrator Status, and Type of Harassment to Outcomes". Journal of Vocational Behavior. 56: 299–329. June 2000 – via doi:10.1006/jvbe.1999.1717.
|first=missing|last=(help) - ↑ Jump up to: 7.0 7.1 Hango, Darcy; Moyser, Melissa (December 17, 2018). "Harassment in Canadian workplaces". Statistics Canada.
- ↑ Wang, Sping; Hayes, Laureen (January 2008). "A Review and Evaluation of Workplace Violence Prevention Programs in the Health Sector Co-Investigators". Nursing Health Services Research Unit: 1–41.
- ↑ Shields, Margot; Wilkins, Kathryn (April 2009). "Factors related to on-the-job abuse of nurses by patients". Component of Statistics Canada Catalogue. 20: 1–14. doi:10.1.1.535.1569 Check
|doi=value (help). line feed character in|title=at position 30 (help) - ↑ Schieder, Jessica (July 20, 2016). ""Women's work" and the gender pay gap". Economic Policy Institute.
- ↑ Gebhard, Roberta (December 05,2017). "#MeTooMedicine". American Medical Women's Association. Check date values in:
|date=(help) - ↑ "Mentoring Women in the Era of #MeTooMedicine". Federation of Medical Women of Canada. October 18, 2018.
|first=missing|last=(help) - ↑ Jump up to: 13.0 13.1 Jagsi, Reshma; Griffith, Kent; Jones, Rochelle (May 17, 2016). "Sexual Harassment and Discrimination Experiences of Academic Medical Faculty". JAMA. 315: 2120–2121. doi:10.1001/jama.2016.2188.
- ↑ Pompilio, Ersilia (January 14, 2020). "Gender Roles In Nursing". Elite healthcare.
- ↑ Jump up to: 15.0 15.1 Renkas, Rebecca R (October 30, 2019). "Female doctors better for health care, but experience gender pay gap, discrimination and depression: U of T expert". University of Toronto.
- ↑ "Canada and the G7". Government of Canada. January 23, 2020.
|first=missing|last=(help)