Documentation:Documentation:FIB book/Non-Contact Anterior Cruciate Ligament (ACL) Injuries in indoor sports.
Original Authors: Fatemeh Nayeri (University of Guelph), Zahra Navardi (University of Guelph), Katelyn Roe (University of Guelph)
Summary
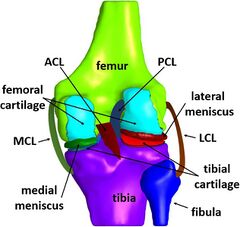
The Anterior Cruciate Ligament (ACL) is one of knee’s four crucial ligaments, which maintains the stability of the knee joint, prevents tibial translations, and limits the rotation [1]. It accounts for up to 86% of the overall resistance against anterior displacement [2]. ACL injuries range from relatively mild, involving the stretching of the ligament's fibers, to more severe injuries including partial or complete ruptures [3]. 10 to 27% of ACL tears are partial and if not taken care of, they can progress to complete rupture [4]. A non-contact ACL injury is one of the most common injuries in sports such as basketball and volleyball, typically resulting from leg cutting, pivoting, or drop landing [5][6]. This review gathers information about non-contact ACL injury in sports, most notably, in basketball and volleyball, which are played on the hard surface of gymnasiums as well as possible prevention and treatment strategies.
Background
Epidemiology
It is estimated that up to 91% of ACL injuries occur during sport, particularly in non-contact instances [7]. Around 200,000 to 250,000 ACL injuries occur annually in the United States alone [8][9][10], resulting in surgical costs exceeding $13,000 USD per procedure [10]. A significant recover and rehabilitation period of at least a 2-year is recommended before resuming pre-injury levels of physical activity [11]. There may be long-term consequences, such as alteration of knee kinematics, associated meniscus, and cartilage damage, and ultimately knee osteoarthritis [12]. It is estimated that one-third of players do not regain their former level of sports participation, and half of them do not resume participation in competitive sports [13][14]. Moreover, for those who return, the overall incidence rate of a second ACL injury within two years after ACL reconstruction, is 15 times greater than healthy athletes [15]. ACL injuries in sport are categorized into contact and non-contact groups, and most of them fall to the latter category for sports such as volleyball and basketball, where up to 70-90% of ACL injuries non-contact instances [5][16][17]. In an epidemiological study of the Italian professional women's volleyball league, it was observed that 97% of ACL ruptures were non-contact [18].
In volleyball, most injuries occurred during games rather than training sessions [6]. There have been ACL injury studies in different sports, especially in soccer or American football, which are played on natural turf . These differences suggest that the context of the sport is an important factor in determining injury, and these must be carefully considered when analyzing and predicting ACL risk.
The probability of ACL tears in female players is 2 to 8 times higher than in male basketball players [5][14][19][20][21]. These injuries are significantly more common within athletes between 21 and 25 years old [18][22].
Biomechanical Mechanisms
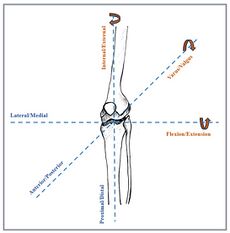
The knee joint can move in six degrees of freedom, which include three translational and three rotational. Rotating about the three principal axes shown in Figure 2. results in internal-external rotation, flexion-extension, and varus-valgus rotation [23]. Non-contact ACL injuries arise from the substantial force or torque produced by the player on their own knee joint surpassing its maximum load-bearing capacity [16]. Landing with excessive varus/valgus, internal/external tibial rotations or with low flexion angles increases the risk of ACL injury. Anterior tibial shear force, mainly from the sagittal and coronal plane, high knee laxity, and excessive force on quadriceps may also lead to this kind of injury [5][16][24]. However, there is not a single mechanism responsible for ACL injury in general, but a combination of several factors which vary from case to case [24].
Causes and risk Factors
Several factors have been found to be associated with increased risk of ACL injuries include body kinematics and kinematics, physiology and anatomy, and external factors.
Body Kinematics and kinetics
75% of ACL injuries in volleyball practices happen during the jump-landing phase [25]. Players who generate force quickly during their jumps tend to experience more force when they land. Additionally, the time it takes to reach the peak power during the jump is also related to the force at landing. Specifically, players who take longer to reach their peak power during a jump tend to experience more force when they land [26]. After some movements such as blocking and spiking in volleyball, players may land on one leg or two, with different knee flexions and tibial positions relative to the femur [6][16][27]. Volleyball players often land on one foot after a spike shot because of the shift in their center of gravity and loss of balance. This may increase non-contact ACL injuries because of higher peak vertical ground reaction force, loading rate, knee valgus angle, and knee flexion moment than both-legs landings [16]. Podraza and White, (2010) found that the knee flexion angle plays a crucial role in the risk of non-contact ACL injuries and that an extended knee landing position with knee flexions between 0° and 25°, poses the highest risk for ACL injuries [28]. This is because the ACL is most in tension when the knee is extended [28][29][30], leading to increased foot–ground impact forces [22][30][31][32][33]. Landing with a more bent knee decreases the ground reaction force as the antigravity muscles are positioned in a way that absorbs the impact’s kinetic energy more [28]. According to a study by DeMorat et al. (2004), excessive quadriceps force at or near knee’s full extension may also contribute to ACL injuries. Using radiographic and mathematical analyses, their cadaveric experiment estimated the maximum isometric quadriceps contraction in a normal person as 3000 N on average, and 6000-7000 N in young, trained male athletes. Applying a force of 4500 N to the quadriceps was sufficient to induce damage to the ACL in all tested knees. This is consistent with a study by Wall et al. (2012), which concluded that the combination of compressive forces and quadriceps load had a synergistic effect [9]. Upon adding a load to the quadriceps, the compressive force required to cause an ACL injury was much lower than when compressive forces were applied alone [34]. Furthermore, abnormal anterior tibial translation, varus and valgus, and internal and external rotation of tibia are other common kinetic factors of ACL injury [5][7][27][30][35][36].
Physiological and Anatomy
Sex differences
Most previous studies agree that women are 2-8 times more susceptible to ACL injuries and this may be because of differences in their anatomical, physiological, and biomechanical features [5][14][17][20][37]. Fluctuating hormones in females, such as estrogen and progesterone may be responsible for the higher rate of ACL injuries in women due to an increase in the knee laxity [38][39][40].
Due to female and male biomechanical differences, the angle between hip and knee is larger in women than in men, which increases the risk of ACL injury risks [41]. However, some studies emphasize movement techniques regardless of players’ sex. In a study implemented on 19 male and 19 female basketball players, it was found that female athletes tend to land with less knee flexion and encounter higher ground reaction forces at the maximum knee flexion compared to their male counterparts during cutting movements. Individual athletes, regardless of gender, demonstrating similar traits, may face an increased risk of ACL injury [42].
Fatigue
Fatigue appears to contribute to ACL injuries by negatively impacting proprioception and altering biomechanics during the demanding phases of volleyball games, particularly during landing [6]. When players are tired, they are more likely to land with a more extended knee which increases the ACL risk injury [43]. As such it is crucial for athletes to rest and avoid over-exertion to minimize injury risk.
External Factors
Landing surface and shoes
Upon landing from a jump, both footwear and the surface naturally dampen a segment of the impact energy [44]. The material deformity and the ability of the landing surface to absorb the impact and prolong the interval time, is an important risk factor. Additionally, surfaces that exhibit a higher friction coefficient with shoes preventing significant sliding and feet’s free rotation, are more likely to contribute to ACL injuries [45][46]. On the other hand, landing on natural and artificial turf allow for greater sliding, which minimizes the joint moments and lower limb injuries [45].
Prevention
There are measures which may be taken to reduce the risk of ACL injuries. It is suggested that athletes participate in prevention programs, 20 to 30 minutes, several times per week [47][48], starting at an early age [49]. Verbal and visual feedback can also be very helpful. If the coach verbally emphasizes during the play that players need to bend their knees as much as they can when landing or if players review their performance in the videos and try to correct their movements and focus on improving their landing mechanics in order to reduce knee valgus collapse and excessive knee rotations [48]. The neuromuscular training is focused on ensuring controlled landing, optimizing absorption of ground reaction force, as well as analysis and progressive feedback, from basic to advanced [42]. The proper use of gluteal muscles, hamstrings, gastrocnemius, and soleus is crucial to control the lower limb and therefore, prevent ACL injuries [6]. Moreover, when knee braces are used, reduction in knee valgus and internal rotation during tasks such as pivoting and single-leg landing may be seen [50] as well as knee extension on landing, and the anterior tibial translation by up to 40% [51]
Treatment
In case of partial and complete tears, conservative treatments such as physiotherapy and special exercises are often leveraged. In most cases, it is accompanied by activity modifications, especially avoiding pivoting [52]. ACL Reconstruction surgery is one of the most common treatment techniques in which an autograft (the transplantation of tissue from one part of an individual's body to another part of the same individual's body) or allograft (The transplantation of tissue from one individual to another individual of the same species) is used to reconstruct the ACL [53]. Many studies have identified the disadvantage of reconstruction surgery by mentioning its serious side effects including meniscal damage, premature osteoarthritis as well as the fact that not all athletes can return to sport after the operation [54]. It is critical for players to be informed about all treatment options during counseling, so that they can decide according to their aims and expectations [55]. Others like Smith et al., in 2014 however, found that functional braces have no effect in improving the injury, but reduces the probability of a second injury [56].
Limitation and future work
One of the most important limitations of this review is the fact that due to the complexity of the knee joint, and due to individualized physical and physiological features, ACL injuries can be attributed to various factors. Moreover, there were considerably fewer studies about ACL injury in women, although they are up to 8 times more susceptible than male athletes. Another limitation was the limited sample size in most studies, which usually affects the accuracy of results. Studies with soft tissue models had the problem of complexity and high cost. There was also a lack of enough studies about prevention techniques and about the link between knee laxity and its impact on ACL injury mechanism. There are also conflicted ideas about the role of internal and external tibial rotation on ACL tear.
In the future, further research on sex differences, computer modeling techniques, prevention methods, the effect of knee laxity as well as internal and external tibial rotation impact are needed. There is also a need to study rehabilitation techniques to avoid surgery or reinjury. In addition, more research is needed on ACL joint loading during normal activities.
References
- ↑ "1. Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N. The anatomy of the ACL and its importance in ACL reconstruction". European Journal of Orthopaedic Surgery and Traumatology. 2013;23(7):747-752. doi:10.1007/s00590-012-1079-8. no-break space character in
|title=at position 4 (help) - ↑ "Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: Is "valgus collapse" a sex-specific mechanism?". Br J Sports Med. 2009;43(5):328-335. doi:10.1136/bjsm.2009.059139.
- ↑ "Odensten, M., Lysholm, J., & Gillquist, J. (1985). The course of partial anterior cruciate ligament ruptures. ". The American Journal of Sports Medicine, 13(3), 183-186.
- ↑ "Fayard JM, Sonnery-Cottet B, Vrgoc G, et al. Incidence and Risk Factors for a Partial Anterior Cruciate Ligament Tear Progressing to a Complete Tear After Nonoperative Treatment in Patients Younger Than 30 Years". Orthop J Sports Med. 2019;7(7). doi:10.1177/2325967119856624.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 5.5 [www.cjsportmed.com "Siegel L, Vandenakker-Albanese C, Siegel D. Anterior Cruciate Ligament Injuries: Anatomy, Physiology, Biomechanics, and Management.; 2012. www.cjsportmed.com"] Check
|url=value (help). Clinical Journal of Sport Medicine 22(4):p 349-355, July 2012. | DOI: 10.1097/JSM.0b013e3182580cd0. - ↑ Jump up to: 6.0 6.1 6.2 6.3 6.4 "Tsarbou C, Liveris NI, Tsimeas PD, Papageorgiou G, Xergia SA, Tsiokanos A. The effect of fatigue on jump height and the risk of knee injury after a volleyball training game: A pilot study". Biomed Hum Kinet. 2021;13(1):197-204. doi:10.2478/bhk-2021-0024.
- ↑ Jump up to: 7.0 7.1 "Meyer EG, Haut RC. Anterior cruciate ligament injury induced by internal tibial torsion or tibiofemoral compression". J Biomech. 2008;41(16):3377-3383. doi:10.1016/j.jbiomech.2008.09.023.
- ↑ Elizabeth Arendt, MD and Randall Dick, MS (November 1995). "Knee Injury Patterns Among Men and Women in Collegiate Basketball and Soccer: NCAA Data and Review of Literature". The American Journal of Sports Medicine. Volume 23, Issue 6.CS1 maint: multiple names: authors list (link)
- ↑ Jump up to: 9.0 9.1 "DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W. Aggressive Quadriceps Loading Can Induce Noncontact Anterior Cruciate Ligament Injury". American Journal of Sports Medicine. 2004;32(2):477-483. doi:10.1177/0363546503258928.
- ↑ Jump up to: 10.0 10.1 "Herzog MM, Marshall SW, Lund JL, Pate V, Spang JT. Cost of Outpatient Arthroscopic Anterior Cruciate Ligament Reconstruction Among Commercially Insured Patients in the United States". 2005-2013. Orthop J Sports Med. 2017;5(1). doi:10.1177/2325967116684776.
- ↑ "Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study". Br J Sports Med. 2016;50(13):804-808. doi:10.1136/bjsports-2016-096031.
- ↑ "Gottlob CA, Baker CL. Anterior cruciate ligament reconstruction: socioeconomic issues and cost effectiveness". Am J Orthop 2000;29:472-6.
- ↑ "Eather N, Wade L, Pankowiak A, Eime R. The impact of sports participation on mental health and social outcomes in adults: a systematic review and the 'Mental Health through Sport' conceptual model". Syst Rev. 2023;12(1). doi:10.1186/s13643-023-02264-8.
- ↑ Jump up to: 14.0 14.1 14.2 "Ardern CL, Ekås G, Grindem H, et al. 2018 International Olympic Committee Consensus Statement on Prevention, Diagnosis, and Management of Pediatric Anterior Cruciate Ligament Injuries". Orthop J Sports Med. 2018;6(3). doi:10.1177/2325967118759953.
- ↑ "Paterno M V., Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport". American Journal of Sports Medicine. 2014;42(7):1567-1573. doi:10.1177/0363546514530088.
- ↑ Jump up to: 16.0 16.1 16.2 16.3 16.4 "Xu D, Jiang X, Cen X, Baker JS, Gu Y. Single-leg landings following a volleyball spike may increase the risk of anterior cruciate ligament injury more than landing on both-legs". Applied Sciences (Switzerland). 2021;11(1):1-14. doi:10.3390/app11010130.
- ↑ Jump up to: 17.0 17.1 "Boden, Barry P., Frances T. Sheehan, Joseph S. Torg, and Timothy E. Hewett. "Non-contact ACL injuries: mechanisms and risk factors."". The Journal of the American Academy of Orthopaedic Surgeons 18, no. 9 (2010): 520.
- ↑ Jump up to: 18.0 18.1 "Devetag F, Mazzilli M, Benis R, La Torre A, Bonato M. Anterior cruciate ligament injury profile in Italian serie A1-A2 women's volleyball league". Journal of Sports Medicine and Physical Fitness. 2018;58(1-2):92-97. doi:10.23736/S0022-4707.16.06731-1.
- ↑ "Cheung EC, Boguszewski D V., Joshi NB, Wang D, McAllister DR. Anatomic Factors that May Predispose Female Athletes to Anterior Cruciate Ligament Injury". Curr Sports Med Rep. 2015;14(5):368-372. doi:10.1249/JSR.0000000000000188.
- ↑ Jump up to: 20.0 20.1 "Montalvo AM, Schneider DK, Yut L, et al. "what's my risk of sustaining an ACL injury while playing sports?" A systematic review with meta-analysis". Br J Sports Med. 2019;53(16):1003-1012. doi:10.1136/bjsports-2016-096274.
- ↑ "Boden, Barry P., Frances T. Sheehan, Joseph S. Torg, and Timothy E. Hewett. "Non-contact ACL injuries: mechanisms and risk factors."". The Journal of the American Academy of Orthopaedic Surgeons 18, no. 9 (2010): 520.
- ↑ Jump up to: 22.0 22.1 "Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: A review of the Hunt Valley II Meeting". January 2005. In: American Journal of Sports Medicine. Vol 34. ; 2006:1512-1532. doi:10.1177/0363546506286866.
- ↑ "Woo, Savio LY, Richard E. Debski, John D. Withrow, and Marsie A. Janaushek. "Biomechanics of knee ligaments."". The American journal of sports medicine 27, no. 4 (1999): 533-543.
- ↑ Jump up to: 24.0 24.1 "Wetters N, Weber AE, Wuerz TH, Schub DL, Mandelbaum BR. Mechanism of Injury and Risk Factors for Anterior Cruciate Ligament Injury". Operative Techniques in Sports Medicine, 24(1), 2-6.
- ↑ "Garcia S, Delattre N, Berton E, Divrechy G, Rao G. Comparison of landing kinematics and kinetics between experienced and novice volleyball players during block and spike jumps". BMC Sports Sci Med Rehabil. 2022;14(1). doi:10.1186/s13102-022-00496-0.
- ↑ "Molla RY, Fatahi A, Khezri D, Ceylan HI, Nobari H. Relationship between impulse and kinetic variables during jumping and landing in volleyball players". BMC Musculoskelet Disord. 2023;24(1). doi:10.1186/s12891-023-06757-4.
- ↑ Jump up to: 27.0 27.1 "Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases". American Journal of Sports Medicine. 2007;35(3):359-367. doi:10.1177/0363546506293899.
- ↑ Jump up to: 28.0 28.1 28.2 "Podraza, J. T., & White, S. C. (2010). Effect of knee flexion angle on ground reaction forces, knee moments and muscle co-contraction during an impact-like deceleration landing: implications for the non-contact mechanism of ACL injury". The Knee, 17(4), 291-295.
- ↑ "Ektas N, Scholes C, Kulaga S, Kirwan G, Lee B, Bell C. Recovery of knee extension and incidence of extension deficits following anterior cruciate ligament injury and treatment: A systematic review protocol". J Orthop Surg Res. 2019;14(1). doi:10.1186/s13018-019-1127-8.
- ↑ Jump up to: 30.0 30.1 30.2 "Boden, B. P., Dean, G. S., Feagin, J. A., & Garrett, W. E. (2000). Mechanisms of anterior cruciate ligament injury". Orthopedics, 23(6), 573-578.
- ↑ "Griffin, L., Albohm, M., Arendt, E., Bahr, R., Beynnon, B., Demaio, M., et al. (2006, September). Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005". American Journal of Sports Medicine, 34(9), 1512–1532.
- ↑ "Lin CF, Liu H, Gros MT, Weinhold P, Garrett WE, Yu B. Biomechanical risk factors of non-contact ACL injuries: A stochastic biomechanical modeling study". J Sport Health Sci. 2012;1(1):36-42. doi:10.1016/j.jshs.2012.01.001.
- ↑ "Leppänen M, Pasanen K, Kujala UM, et al. Stiff Landings Are Associated with Increased ACL Injury Risk in Young Female Basketball and Floorball Players". American Journal of Sports Medicine. 2017;45(2):386-393. doi:10.1177/0363546516665810.
- ↑ "Wall, S. J., Rose, D. M., Sutter, E. G., Belkoff, S. M., & Boden, B. P. (2012). The role of axial compressive and quadriceps forces in noncontact anterior cruciate ligament injury: a cadaveric study". The American journal of sports medicine, 40(3), 568-573.
- ↑ "Kiapour AM, Quatman CE, Goel VK, Wordeman SC, Hewett TE, Demetropoulos CK. Timing sequence of multi-planar knee kinematics revealed by physiologic cadaveric simulation of landing: Implications for ACL injury mechanism". Clinical Biomechanics. 2014;29(1):75-82. doi:10.1016/j.clinbiomech.2013.10.017.
- ↑ "Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: Is "valgus collapse" a sex-specific mechanism?". Br J Sports Med. 2009;43(5):328-335. doi:10.1136/bjsm.2009.059139.
- ↑ "Cheung EC, Boguszewski D V., Joshi NB, Wang D, McAllister DR. Anatomic Factors that May Predispose Female Athletes to Anterior Cruciate Ligament Injury". Curr Sports Med Rep. 2015;14(5):368-372. doi:10.1249/JSR.0000000000000188.
- ↑ "Konopka JA, Hsue L, Chang W, Thio T, Dragoo JL. The Effect of Oral Contraceptive Hormones on Anterior Cruciate Ligament Strength". American Journal of Sports Medicine. 2020;48(1):85-92. doi:10.1177/0363546519887167.
- ↑ "Liu SH, Al-Shaikh R, Panossian V, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament". Journal of Orthopaedic Research. 1996;14(4):526-533. doi:10.1002/jor.1100140405.
- ↑ "Deie M, Sakamaki Y, Sumen Y, Urabe Y, Ikuta Y. Anterior knee laxity in young women varies with their menstrual cycle". Int Orthop. 2002;26(3):154-156. doi:10.1007/s00264-001-0326-0.
- ↑ "Hughes, G., & Watkins, J. (2006). A risk-factor model for anterior cruciate ligament injury". Sports Medicine, 36, 411-428.
- ↑ Jump up to: 42.0 42.1 "James LP, Kelly VG, Beckman EM. Injury risk management plan for volleyball athletes". Sports Med. 2014;44(9):1185-1195. doi:10.1007/s40279-014-0203-9.
- ↑ "McLean SG, Samorezov JE. Fatigue-induced acl injury risk stems from a degradation in central control". Med Sci Sports Exerc. 2009;41(8):1661-1672. doi:10.1249/MSS.0b013e31819ca07b.
- ↑ "Bruce OL, Firminger CR, Wannop JW, Stefanyshyn DJ, Edwards WB. Effects of basketball court construction and shoe stiffness on countermovement jump landings". Footwear Sci. 2019;11(3):171-179. doi:10.1080/19424280.2019.1668867.
- ↑ Jump up to: 45.0 45.1 "Nigg, B. M., Stefanyshyn, D. J., Rozitis, A. I., & Mündermann, A. (2009). Resultant knee joint moments for lateral movement tasks on sliding and non-sliding sport surfaces". Journal of sports sciences, 27(5), 427-435.
- ↑ "Chivers, I. H., Aldous, D. E., & Orchard, J. W. (2005). The relationship of Australian football grass surfaces to anterior cruciate ligament injury". The relationship of Australian football grass surfaces to anterior cruciate ligament injury., 10, 327-332.
- ↑ "Sadoghi P, Von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs". Journal of Bone and Joint Surgery. 2012;94(9):769-776. doi:10.2106/JBJS.K.00467.
- ↑ Jump up to: 48.0 48.1 "Joy, E. A., Taylor, J. R., Novak, M. A., Chen, M., Fink, B. P., & Porucznik, C. A. (2013). Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches". The Journal of Strength & Conditioning Research, 27(8), 2263-2269.
- ↑ "Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: A meta-analysis". American Journal of Sports Medicine. 2013;41(1):203-215. doi:10.1177/0363546512460637.
- ↑ "Hanzlíková, I., Richards, J., Tomsa, M., Chohan, A., May, K., Smekal, D., & Selfe, J. (2016). The effect of proprioceptive knee bracing on knee stability during three different sport related movement tasks in healthy subjects and the implications to the management of Anterior Cruciate Ligament (ACL) injuries". Gait & posture, 48, 165-170.
- ↑ "LaBella, C. R., Hennrikus, W., Hewett, T. E., Council on Sports Medicine and Fitness, and Section on Orthopaedics, Brenner, J. S., Brookes, M. A., ... & Wells, L. (2014). Anterior cruciate ligament injuries: diagnosis, treatment, and prevention". Pediatrics, 133(5), e1437-e1450.
- ↑ "Strehl A, Eggli S. The value of conservative treatment in ruptures of the anterior cruciate ligament (ACL)". Journal of Trauma - Injury, Infection and Critical Care. 2007;62(5):1159-1162. doi:10.1097/TA.0b013e31805006e7.
- ↑ "Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: Principles of treatment". EFORT Open Rev. 2016;1(11):398-408. doi:10.1302/2058-5241.1.160032.
- ↑ "Delincé P, Ghafil D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature". Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(1):48-61. doi:10.1007/s00167-011-1614-x.
- ↑ "Ferretti, A., Papandrea, P., Conteduca, F., & Mariani, P. P. (1992). Knee ligament injuries in volleyball players". The American journal of sports medicine, 20(2), 203-207.
- ↑ "Smith SD, LaPrade RF, Jansson KS, Årøen A, Wijdicks CA. Functional bracing of ACL injuries: Current state and future directions". Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(5):1131-1141. doi:10.1007/s00167-013-2514-z.