Course:MEDG550/Student Activities/ Beta Thalassemia
Beta-thalassemia is a genetic blood condition that affects the production of a protein called hemoglobin [1]. Hemoglobin is found in red blood cells and plays an important role in transporting oxygen around the body [1]. Beta-thalassemia is common in individuals from certain parts of the world. It is most common in people who are from Southeast Asia, the Middle East, North and Central Africa, Central Asia, and the Mediterranean[2]. Beta-thalassemia is particularly prevalent in Sardinia and Cyprus [2].
What Causes Beta-thalassemia? Genetics and the HBB Gene
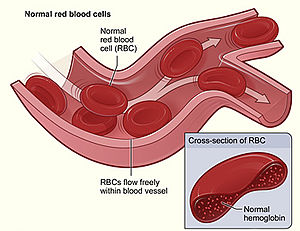
The human body is made up of trillions of cells. Inside each cell, there are structures called chromosomes, which is where the DNA is stored. Different segments of the DNA make up different genes. Genes are important because they provide instructions to make different proteins. Each protein has a unique role that helps the body function properly on a day-to-day basis. One important protein that the body makes is called hemoglobin, which is found inside the body’s red blood cells.[1] Hemoglobin is made up of four different units that are bound together.[1] Two of the units are called “alpha” and two of the units are called “beta”.[1] Hemoglobin plays an important role in transporting oxygen around the body and delivering it to the body’s tissues.[1]
Beta-thalassemia is caused by spelling mistakes or “variants” in the HBB gene, which makes the beta unit of hemoglobin.[2] Variants in the HBB gene can have different effects. Some variants lead to not enough beta units being produced, while other variants lead to no beta units being produced altogether.[3] This is a problem because the beta and alpha units need to bind together to make hemoglobin.[1] When not enough beta units are made, the alpha units have nothing to bind. As a result, there are too many alpha units, which leads to the alpha units joining together.[1] This damages the body’s red blood cells and leads to the body not having enough healthy red blood cells to transport oxygen around the body (anemia).[1]
What are the Symptoms of Beta-thalassemia?
There are three main forms of beta-thalassemia: beta-thalassemia major, intermedia, and minor.[2] Many different changes or variants in the HBB gene can cause beta-thalassemia.[1] What form of beta-thalassemia someone has depends on the specific type of variant that is found in the HBB gene.[3]
Beta-thalassemia Major
Beta-thalassemia major, also called Cooley’s anemia or Mediterranean Anemia, is the most severe form of beta-thalassemia.[2][3] Individuals who have this type of beta-thalassemia generally first show symptoms in infancy or in the toddler stage of life around 6-24 months.[2] [3] The following symptoms are typically seen in individuals with beta-thalassemia major:
- A significantly decreased amount of healthy red blood cells (severe anemia)[2] [3]
- Skin that becomes more pale with time[2] [3]
- Delayed physical growth in infants (failure to thrive)[2] [3]
- Difficulties with feeding as an infant [2] [3]
- Diarrhea[2] [3]
- An increase in the size of the belly due to enlargement of the spleen[2] [3]
- Frequent infections and fevers[2] [3]
Infants and toddlers with beta-thalassemia major require immediate management to control their symptoms. Without proper management, individuals with beta-thalassemia major may also experience the following symptoms:
- Yellowing of the skin (jaundice)[2][3]
- The formation of open sores on the legs[2][3]
- Slowed growth[2][3]
- Swelling of the liver and the spleen[2][3]
- Reduced muscle tone[2][3]
- Alterations to the shapes of the bones of the legs and face[2][3]
- Weakening of the bones (osteoporosis)[2][3]
- The formation of bone masses[3]
- A condition where the knees turn inwards (Genu Valgum)[2][4]
Beta-thalassemia Intermedia
Beta-thalassemia intermedia is a less severe form of beta-thalassemia than beta-thalassemia major.[3] Individuals with beta-thalassemia intermedia tend to develop symptoms later in life compared to those with beta-thalassemia major.[3] Some people with beta-thalassemia intermedia may not even develop symptoms until adulthood.[3] Common features of beta-thalassemia intermedia are:
- Milder form of anemia[2][3]
- Yellowing of the skin (jaundice)[2][3]
- Skin that is paler than normal[2][3]
- Formation of stones in the gallbladder[2]
- Development of open sores on the legs[2][3]
- Swelling of the liver and the spleen[2][3]
- Increased chance of developing weak bones[2][3]
Beta-thalassemia Minor
Beta-thalassemia minor is also referred to as beta-thalassemia trait, beta-thalassemia carrier, or heterozygous beta-thalassemia.[3] Individuals who have beta-thalassemia minor generally do not experience any symptoms.[2][3] However, sometimes people with beta-thalassemia minor may have mild anemia.[2][3]
Secondary Complications
In addition to the symptoms discussed above, individuals with beta-thalassemia major or intermedia are also at risk of developing further complications related to having too much iron in their body.[2][3] Iron is a mineral that is found in hemoglobin and helps the hemoglobin protein transport oxygen around the body.[1] Although the body needs iron, having too much iron can cause problems and lead to iron overload. Iron overload is a condition where iron builds up in the body and is stored in the body’s organs, which causes them to not function properly.[5] Individuals with beta-thalassemia major and intermedia are at risk of iron overload because their gut absorbs too much iron.[3] Additionally, one of the main treatments for beta-thalassemia involves blood transfusions (see management section below).[2][3] Regular blood transfusions can also cause iron overload.[2][3] Symptoms related to iron overload include:
- Scarring of the liver[2][3]
- Liver disease[3]
- Abnormal heart rhythms[3]
- An enlarged heart and heart failure[3]
- Poor growth in children[2][3]
- Delayed puberty in children[2][3]
- Diabetes[2][3]
- Problems with the body's ability to produce hormones[3]
Thankfully, there are treatments available to help reduce the build-up of iron in individuals with beta-thalassemia.
How is Beta-thalassemia Inherited?
Beta-thalassemia runs through families in an autosomal recessive fashion.[2] Everyone has two copies of the HBB gene; one copy is received from your mom while the other copy is received from your dad. For someone to have beta-thalassemia major or intermedia, both copies of their HBB gene must not be working properly.[2] Sometimes, people have one copy of the HBB gene that works properly and one copy that does not. These people are referred to as “carriers” and have beta-thalassemia minor.[2] As discussed above, people with beta-thalassemia minor are generally healthy and do not experience any symptoms of beta-thalassemia.[2][3]
| Form of Beta-thalassemia | Changes in the HBB gene |
|---|---|
| Beta-thalassemia Major | Both copies of the HBB gene do not work properly because they both have a change (variant) in them |
| Beta-thalassemia Intermedia | Both copies of the HBB gene do not work properly because they both have a change (variant) in them |
| Beta-thalassemia Minor | Only one copy of the HBB gene has a change (variant) in it that causes it not to work properly |
When a carrier has a child, there is a 50% chance that the copy of the HBB gene that does not work properly will be passed down to their child.[2] Therefore, when two carriers have a child together, there are three potential outcomes for each pregnancy:
- 25% chance that both parents will pass down the copy of the HBB gene that does not work properly. In this case, the child will have either beta-thalassemia major or intermedia.[2]
- 50% chance that only one of the parents will pass down the copy of the HBB gene that does not work properly. In this case, the child will be a carrier and have beta-thalassemia minor.[2]
- 25% chance that both parents will pass down the copy of the HBB gene that works properly. In this case, the child will not have beta-thalassemia major, intermedia, or minor.[2]
How is Beta-thalassemia Diagnosed?
If a healthcare professional suspects that someone may have beta-thalassemia, they may order a blood test. The blood test is used to look at the size of the red blood cells and the amount of hemoglobin that is present in the blood to help make a diagnosis.[2] A diagnosis of beta-thalassemia is made if the blood test reveals the following four findings:
- Small and pale red blood cells (microcytic hypochromic anemia).[2][3]
- Red blood cells that vary in their sizes and shapes (anisopoikilocytosis nucleated red blood cells).[2][3]
- Very low amounts of none of the hemoglobin protein that is found in adults.[2][3]
- Increased levels of another form of hemoglobin that is typically found in developing babies in the womb called Hemoglobin F.[2]
In babies that are less than 12 months in age, genetic testing may also be done to help make a diagnosis.[2] With genetic testing, the HBB gene is read to look for variants that prevent it from working properly. Genetic testing of the HBB gene is very accurate and detects almost 100% of changes in the gene.[2]
How is Beta-thalassemia Treated?
Fortunately, there are many forms of treatment that can help improve symptoms and the quality of life of individuals with beta-thalassemia.
Management:
Blood Transfusion Therapy:
The main goal of treatment is to help ensure that the body has enough healthy red blood cells.[2][3] This is achieved through regular blood transfusions.[2][3] Blood transfusions are a simple procedure where an individual is given donated blood through a needle in the arm. It is recommended that individuals with beta-thalassemia major receive blood transfusion every two to three weeks.[2] Individuals with beta-thalassemia intermedia may never need a blood transfusion or may only need one on an occasional basis.[3]
Iron Chelation Therapy:
Iron chelation therapy is a form of treatment that removes excess iron from the body.[3] Iron chelators are drugs that bind to iron to form complexes.[6]The iron containing complexes are then removed from the body through urine.[6] It is especially important that individuals with beta-thalassemia who are receiving blood transfusions also undergo iron chelation therapy at the same time. This helps prevent the symptoms caused by iron overload.[2][3] There are many different types of iron chelators, which can be taken as either a pill or injected through a vein in the arm (intravenous administration).[2][3]
Removal of the Spleen:
In some people with beta-thalassemia, the spleen becomes overactive or so large that it could rupture.[3] In these cases, the spleen may be surgically removed.[3]
Hydroxyurea Treatment:
Hydroxyurea is type of medication that increases the amount of another type of hemoglobin in the blood called hemoglobin F.[7] Hemoglobin F is different from the type of hemoglobin that does not work properly in individuals with beta-thalassemia. Because of this, it has been found to improve some symptoms of individuals with beta-thalassemia.[2]
Transplantation:
A bone marrow transplant is the only form of treatment available today that can cure beta-thalassemia.[3] A bone marrow transplant involves giving individuals with beta-thalassemia special cells called stem cells from a donor through an IV in the arm.[8] These stem cells have a copy of the HBB gene that works properly and will make healthy red blood cells in individuals with beta-thalassemia.[8]
Monitoring and Surveillance:
Monitoring For Too Much Iron:
It is important that individuals with beta-thalassemia are closely followed to ensure that their body does not have too much iron. This may include:
- Regular blood tests to measure the amount of iron in the body.[2][7]
- A liver biopsy – a procedure where a doctor removes a small piece of liver tissue using a small needle[2]
- Measuring the amount of iron in the heart or liver using an MRI.[2][7]
Surveillance:
Because beta-thalassemia can require life-long treatment, it is important that people with this condition see their doctor regularly to ensure that their treatment is working properly and to monitor for side-effects of treatment.[2] Regular surveillance may include the following:
| Frequency of Surveillance | Type of Surveillance |
|---|---|
| Every Month |
|
| Every Three Months | |
| Every Year |
Lifestyle Changes:
It is recommended that people with beta-thalassemia make the following changes to their lifestyle:
- Avoid taking iron supplements[2]
- Avoid drinking alcohol- this is especially important for individuals with beta-thalassemia who have liver disease because drinking alcohol can make their liver disease worse.[2]
Genetic Counselling
Individuals who previously had a child with beta-thalassemia, have beta-thalassemia themselves, or are a carrier of this condition may be referred to genetic counselling. Genetic counsellors are healthcare professionals that can help determine someone’s risk of having a child with beta-thalassemia. They can also discuss and provide information about carrier screening, prenatal diagnosis, and family planning. Genetic counsellors also provide emotional support to individuals as they adapt to a diagnosis of beta-thalassemia.
Carrier Screening:
Carrier screening is used to determine if someone has one copy of the HBB gene that does not work properly (individuals that have beta-thalassemia minor). A simple blood test that looks at the shape, size, and amount of hemoglobin can help determine if someone is a carrier.[9] If someone is determined to be a carrier based on a blood test, further genetic testing of the HBB gene may be done.[2] Genetic testing involves reading the HBB gene to look for changes (variants) that prevent it from working properly.[2]
Who is eligible for carrier screening?
Carrier screening is currently offered to:
- Individuals who are part of a high-risk ethnic group.[9] This includes individuals from the following regions: the Middle East, North and West Africa, Southeast Asia, the Mediterranean, and Central Asia.[2][9]
- Individuals who are related to someone with beta-thalassemia.[2]
- Individuals whose partner is a carrier for beta-thalassemia.[9]
- Individuals who used a sperm or egg donor for their pregnancy[2]
Family Planning:
If both members of a couple are carriers for beta-thalassemia, they can talk to a genetic counsellor to determine the chances that they have a child with beta-thalassemia major or intermedia in the future. If both members of a couple are carriers, there is a 25% chance of having a child with beta-thalassemia major or intermedia with each pregnancy.[2]
Prenatal Testing and Preimplantation Genetic Diagnosis:
Couples that have a chance of having a child with beta-thalassemia major or intermedia can choose to undergo prenatal diagnosis or preimplantation genetic diagnosis. Both prenatal testing/diagnosis and preimplantation genetic diagnosis are typically done after both members of the couple undergo genetic testing to determine the exact change in the HBB gene.[2]
Prenatal Testing:
Prenatal testing involves testing the DNA from the developing baby to see if the baby has beta-thalassemia major or intermedia.[10] There are two options for prenatal diagnosis:
- Amniocentesis: Involves inserting a fine needle through the belly and removing some of the fluid that surrounds the baby in the womb.[1][10] Women typically undergo this procedure around weeks 15-18 of their pregnancy.[10]
- Chorionic Villus Sampling: A fine needle is inserted either through the belly or cervix to remove a small piece of tissue from the placenta.[1][10] Women typically undergo this procedure around weeks 11-13 of their pregnancy.[10]
Preimplantation Genetic Diagnosis:
Before a couple gets pregnant, a couple can chose to undergo IVF. During IVF, egg cells are removed from the female partner and sperm cells are collected from the male partner.[1] The sperm and egg cells are then combined in a dish to create an embryo.[1] The embryo can then be tested to see if it has variants in the HBB gene. Couples can choose to use an embryo that does not have beta-thalassemia to be placed inside the womb.
Psychosocial Implications:
A diagnosis of beta-thalassemia may impact individuals and families in emotional ways. For some individuals, beta-thalassemia requires lifelong treatment from a young age.[11] Children with beta-thalassemia may frequently miss school for treatment and parents may find it emotionally challenging to cope with the demands of caring for a child with complex medical needs.[11] The rigorous treatment plans may make it difficult for some individuals to cope with them, especially considering many of the treatments have negative side effects.[11] Furthermore, some individuals with beta-thalassemia may experience severe and life-threatening complications, which may shorten their life expectancy.[11] It is common for individuals and families to experience anxiety, depression, and feelings of uncertainty over not knowing what the future may hold.[11] Each individual and family living with a diagnosis of beta-thalassemia may experience unique psychological concerns. Talking to a genetic counsellor or another healthcare professional may help individuals and families cope with a diagnosis and help provide connections to resources in the community.
Patient Resources
The following links provide more information and resources for individuals and families affected by beta-thalassemia.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 Nussbaum, Robert L.; McInnes, Roderick R.; Willard, Huntington F. (2015). Thompson & Thompson Genetics in Medicine (E-Book) (8th ed.). Elsevier Health Sciences.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 2.34 2.35 2.36 2.37 2.38 2.39 2.40 2.41 2.42 2.43 2.44 2.45 2.46 2.47 2.48 2.49 2.50 2.51 2.52 2.53 2.54 2.55 2.56 2.57 2.58 2.59 2.60 2.61 2.62 2.63 2.64 2.65 2.66 2.67 2.68 2.69 2.70 2.71 2.72 2.73 2.74 2.75 2.76 2.77 2.78 2.79 2.80 Origa, Raffaella. Beta-Thalassemia. 2000 Sep 28 [Updated 2021 Feb 4]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1426/
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 3.28 3.29 3.30 3.31 3.32 3.33 3.34 3.35 3.36 3.37 3.38 3.39 3.40 3.41 3.42 3.43 3.44 3.45 3.46 3.47 3.48 3.49 3.50 3.51 3.52 3.53 3.54 3.55 Origa R. β-Thalassemia. Genetics in Medicine. 2017 Jun;19(6):609-619. doi: 10.1038/gim.2016.173. Epub 2016 Nov 3. PMID: 27811859.
- ↑ Patel M, Nelson R. Genu Valgum. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559244/
- ↑ Muncie HL Jr, Campbell J. Alpha and beta thalassemia. American Family Physician. 2009 Aug 15;80(4):339-44. PMID: 19678601.
- ↑ 6.0 6.1 Mobarra N, Shanaki M, Ehteram H, Nasiri H, Sahmani M, Saeidi M, Goudarzi M, Pourkarim H, Azad M. A Review on Iron Chelators in Treatment of Iron Overload Syndromes. Int J Hematol Oncol Stem Cell Res. 2016 Oct 1;10(4):239-247. PMID: 27928480; PMCID: PMC5139945.
- ↑ 7.0 7.1 7.2 Khandros E, Kwiatkowski JL. Beta Thalassemia: Monitoring and New Treatment Approaches. Hematol Oncol Clin North Am. 2019 Jun;33(3):339-353. doi: 10.1016/j.hoc.2019.01.003. Epub 2019 Apr 2. PMID: 31030806.
- ↑ 8.0 8.1 Thalassaemia International Federation (2018). "BONE MARROW TRANSPLANTATION (BMT) in β-thalassaemia" (PDF). Retrieved January 20th, 2022. line feed character in
|title=at position 28 (help); Check date values in:|access-date=(help) - ↑ 9.0 9.1 9.2 9.3 Wilson RD, De Bie I, Armour CM, Brown RN, Campagnolo C, Carroll JC, Okun N, Nelson T, Zwingerman R, Audibert F, Brock JA, Brown RN, Campagnolo C, Carroll JC, De Bie I, Johnson JA, Okun N, Pastruck M, Vallée-Pouliot K, Wilson RD, Zwingerman R, Armour C, Chitayat D, De Bie I, Fernandez S, Kim R, Lavoie J, Leonard N, Nelson T, Taylor S, Van Allen M, Van Karnebeek C. Joint SOGC-CCMG Opinion for Reproductive Genetic Carrier Screening: An Update for All Canadian Providers of Maternity and Reproductive Healthcare in the Era of Direct-to-Consumer Testing. J Obstet Gynaecol Can. 2016 Aug;38(8):742-762.e3. doi: 10.1016/j.jogc.2016.06.008. PMID: 27638987.
- ↑ 10.0 10.1 10.2 10.3 10.4 Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010 May 21;5:11. doi: 10.1186/1750-1172-5-11. PMID: 20492708; PMCID: PMC2893117.
- ↑ 11.0 11.1 11.2 11.3 11.4 Behdani F, Badiee Z, Hebrani P, Moharreri F, Badiee AH, Hajivosugh N, Rostami Z, Akhavanrezayat A. Psychological Aspects in Children and Adolescents With Major Thalassemia: A Case-Control Study. Iran J Pediatr. 2015 Jun;25(3):e322. doi: 10.5812/ijp.25(3)2015.322. Epub 2015 Jun 27. PMID: 26199704; PMCID: PMC4505986.