Course:MEDG550/Student Activities/Loeys-Dietz syndrome
Overview
The genetic cause of Loeys-Dietz syndrome (LDS) was recently discovered in 2005 by Dr. Bart Loeys and Dr. Harry Dietz. Characteristics of LDS include a changed appearance to the face and to the skin, bone abnormalities, and most significantly, weakened walls of arteries that lead to the formation of aneurysms and/or blood vessel dissections. The most common cause of death in people with LDS is through a ruptured aneurysm or dissection of the aorta.[1][2] Since the initial description of LDS, mutations in four genes, TGFBR1, TGFBR2, SMAD3, and TGFB2, have been found to cause LDS.[3][4][5][6]
Disease-causing variants in TGFBR1, TGFBR2, SMAD3, or TGFB2 all lead to increased signalling in a protein called 'transforming growth factor β' (TGFβ). TGFβ has many important roles in cell growth, controlled cell death and maintaining cell functions. TGFβ is active throughout development and adulthood. LDS is in a group of conditions with similar disease characteristics called connective tissue disorders, as altered signalling in TGFβ changes the cellular composition of connective tissue.[7][8]
Disease Characteristics
LDS is a genetic condition, meaning that patients with LDS have had the causative genetic variant since before they were born. However, this does not mean patients will have every disease feature present from birth. The clinical presentation, or the features of LDS identified by doctors, varies from patient to patient, even within the same family. The severity of each feature varies as well as the characteristic being present or absent. Historically the disease characteristics of LDS have been classified into two categories, Type I and Type II, depending on the presence (Type I) or absence (Type II) of craniofacial features. In 2014, Drs. Loeys and Dietz proposed changing the classification system to have four categories (Types I - IV) based on the genetic cause of each patient's LDS instead of the disease characteristics present.[3] Both systems of classification are still in use depending on the literature source.
While disease-causing variants in all four genes lead to LDS, some disease characteristics may be more common in one type compared to another. For example, it is suspected that osteoarthritis is more common in Type III LDS (caused by variants in SMAD3) and that dissections of the aorta at an early age are more likely to happen with Type I and Type II LDS (caused by variants in TGFBR1 and TGFBR2, respectively).[9]
Craniofacial
Craniofacial characteristics refer to the features of LDS that involve the shape and/or appearance of the face. Craniofacial characteristics are present in about 75% of LDS patients.[9]
| Medical Term | Description |
|---|---|
| Hypertelorism | Hypertelorism mean that the eyes are farther apart than would be expected for a persons age and sex. |
| Cleft palate | The palate, also called the roof of the mouth, is formed by two structures called the palatine shelves that move upwards within the oral cavity to a horizontal position where they fuse together. This processes separates the mouth from the nasal cavity. A cleft palate occurs when the two palatine shelves fail to fuse together leaving a connection between the oral and nasal cavities. In LDS the cleft palate can also be submucosal, meaning that the skin lining the mouth cavity is covering the opening caused by the cleft palate. |
| Abnormal uvula | The uvula is the single small piece of tissue that hangs at the back of the mouth before the start of the throat. In LDS the uvula can be wider than expected and be bifid, meaning there is a small divide up the centre, or raphe, meaning there is an indentation up the centre of the uvula caused by the two pieces of a bifid uvula fusing together. |
| Craniosynostosis | At a very young age the bones of the skulls are not fully fused together to allow the brain and head to continue to grow. The lines along which the bones eventually fuse are called sutures. When a baby has one or more sutures fused prematurely, or earlier than it should, it is called craniosynostosis. Early fusing of sutures does not prevent the brain from continuing to grow, resulting in an abnormal head shape. |
| Malar hypoplasia | Malar hypoplasia is a term used to describe underdeveloped cheek bones. |
| Retrognathia | Retrognathia describes when the lower part of the mouth (the jaw bone) does not extend out horizontally to meet the upper part of the mouth. People with retrognathia have an "overbite." |
| Developmental delay | This is an uncommon characteristic and rarely appears in LDS patients without other craniofacial features, which indicates that the developmental delay may be an outcome of the structural abnormalities of the head. |
Skin
| Medical Term | Description |
|---|---|
| Velvety skin | Velvety skin refers to skin that feels soft or velvety. |
| Translucent skin | People with LDS have skin that is thinner and more translucent, making the veins below the skin easier to see than in people without LDS or other connective tissue disorders. |
| Abnormal scarring | People with LDS who are wounded will usually take longer to heal and have a much larger scar than would be expected in someone without LDS or other connective tissue disorders. |
| Easy bruising | Due to the fragility of their skin and blood vessels people with LDS bruise more easily than people without LDS or other connective tissue disorders. |
Skeletal
Skeletal characteristics include those that involve the bones and tissues involved in joint function.
| Medical Term | Description |
|---|---|
| Arachnodactyly | Arachnodactyly is a term used to describe fingers and/or toes that are slender and longer than expected for the relative size of the rest of the hand or foot. |
| Pectus deformity | A pectus deformity affects the bones of the chest on the front of the body, namely the rib cage and sternum. People with LDS can have pectus excavatum (where the rib cage appears sunken) or pectus carinatum (where the rib cage appears to be protruding outwards). |
| Scoliosis | Scoliosis is a general term that describes the abnormal curving of the spine to the left or right. About 50% of LDS patients have scoliosis that can range from mild to severe, and can be progressive. |
| Joint hypermobility | People with LDS may have joints with an increased range of motion. This is referred to as joint hypermobility. |
| Joint contractures | In addition to joint hypermobility, people with LDS may be born with restrictions in joint movement called contractures. Camptodactyly, permanent bending of the fingers, is one of the most common types of contractures in LDS. |
| Congenital spine abnormalities | Congenital means that the abnormalities in the spine bones, called vertebrae, have been present since birth. |
| Osteoarthritis | Osteoarthritis is a type of bone inflammation that weakens the bone. LDS patients with osteoarthritis have an increased number of fractures that take longer to heal than usual. |
Cardiovascular
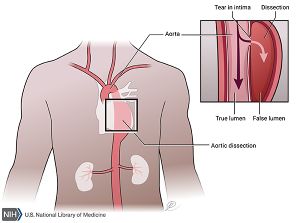
Cardiovascular characteristics are the most frequently seen in LDS and include both abnormalities of the heart and arteries throughout the body. Aneurysms, sack-like outpocketings of blood vessel walls or an increase in the blood vessel diameter, as well as dissections, where the blood vessel wall splits apart, are most frequently seen on the aorta, and are the primary cause of death for LDS patients. People with LDS frequently have multiple blood vessel anomalies (for example, numerous aneurysms throughout the body, or both arterial tortuosity and aneurysms throughout the body).
| Medical Term | Description |
|---|---|
| Aortic-root aneurysm | The aortic-root refers to where the aorta joins the heart. Blood being pumped to the rest of the body from the heart passes through the aortic root at high blood pressure. |
| Peripheral aneurysms | Peripheral aneurysms are sack-like protrusions or diameter increases of arteries in the extremities of the body. This term is often used to described aneurysms that are located outside of the aorta. |
| Arterial tortuosity | Arterial tortuosity is the twisting of arteries, similar to how a corkscrew appears. Arterial tortuosity occurs most frequently in the head or neck, but can occur anywhere in the body. |
| Atrial septal defect | An atrial septal defect is a hole in the septum, or wall, between two chambers of the heart, the right and left atrium. |
| Patent ductus arteriosus | The ductus arteriosus is a blood vessel that comes from the heart and is important in helping transport oxygenated blood from the heart to the rest of the body during development in the uterus. The ductus arteriosus usually closes after birth. A patent ductus arteriosus is one that remains open and functional after birth. |
| Mitral valve prolapse | The mitral valve is a valve that separates two chambers of the heart, the left atrium and left ventricle. A prolapsed mitral valve is one that does not close completely and the pieces of the valve end up in the left atrium instead of the left ventricle. |
Ocular
Ocular characteristics are changes to the eye that may or may not affect vision.
| Medical Term | Description |
|---|---|
| Blue sclerae | This term describes the when the sclerae, the part of the eyeball that is usually white, has a bluish or grey hue. While this feature does not affect eye function, it is in distinguishing LDS from other connective tissue syndromes. |
| Strabismus | A strabismus is when the eyes aren't aligned and point in different directions, for example, one eye may by looking straight ahead while the other eye is looking down and to the right. |
| Myopia | Myopia is a type of vision loss where objects in the distance appear blurry. |
Other
| Medical Term | Description |
|---|---|
| Allergies & immune responses | An immune response occurs when the body comes in contact with a substance it views as harmful to the body. Appropriate immune responses occur when the body comes in contact with harmful viruses or bacteria. Inappropriate immune responses occur when the body comes into a neutral or beneficial substance such a food, and causes an allergic reaction. Allergic reactions to food may present as severe and life threatening, called anaphylaxis, or an ongoing discomfort in the digestive tract, that while not life threatening, can lead to issues in absorbing nutrients from food. In addition to food allergies, people with LDS are more likely to have other inappropriate immune responses such as asthma (lung inflammation), eczema (skin inflammation, often red and itchy), and sinus inflammation. |
Genes and Inheritance
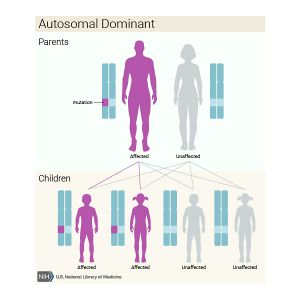
Currently, disease causing variants in four genes TGFBR1, TGFBR2, SMAD3, and TGFB2 are known to cause LDS. People without LDS have two functioning copies of each of these genes. A person has LDS when one of the two copies of TGFBR1, TGFBR2, SMAD3, or TGFB2 carries a disease causing variant that stops the gene from functioning properly. Although some disease characteristics are more frequently seen depending on which gene contains the variant (see Disease Characteristics), it is not possible to predict the severity of LDS based on the specific variant or gene.
In about 25% of patient with LDS the causative variant has been inherited from a parent. In about 75% of patients with LDS the causative variant occurred spontaneously very early in development and was not inherited from a parent.
People with LDS have an equal chance of passing on functioning or non-functioning gene (carrying the disease causing variant) to their children. Both boys and girls have an equal chance of inheriting the disease causing variant, meaning a person with LDS has a 50% chance of passing on LDS to their child.
Diagnosis
LDS is diagnosed through clinical examination and, in some cases, genetic testing. In patients without the craniofacial characteristics of LDS it can be difficult to differential between LDS and other connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome. Also patients with different connective tissue disorders may have the same disease characteristics, it is important to distinguish between these conditions and make an accurate diagnosis as management guideline are different between conditions.
Genetic Testing
In patients where the clinical pictures does match LDS conclusively, genetic testing can be used to look for a disease-causing variant in the four LDS genes. Genetic testing for LDS is often done using a gene panel that sequences genes related to other connective tissue disorders in addition to TGFBR1, TGFBR2, SMAD3, and TGFB2. If a disease-causing variant is found in TGFBR1, TGFBR2, SMAD3, and TGFB2 then a genetic diagnosis of LDS will be made.
Management
LDS patients are cared for by a multidisciplinary team of specialists including geneticists (doctors specializing in genetic conditions), cardiologists (heart doctors and surgeons), ophthalmologists (eye doctors) and orthopedists (doctors of the skeletal system). It is recommended to see a geneticist and/or a genetic counsellor around the time of diagnosis to facilitate genetic testing and screening decisions for family members (See Genetic Counselling). This initial visit with the genetics specialists is also important for coordinating care with other specialists the patient may not have seen or been referred to yet.
All LDS patients will need to have non-invasive imagining, such as MRI, regularly to look at the arteries throughout the body. Although the aorta is the most likely blood vessel to be affected, about 50% of LDS patients have aneurysms located elsewhere in the body such as the arms, brain, and organs. Full body imaging for cardiovascular symptoms should be conducted to detect new aneurysms or dilations, and to monitor already identified cardiovascular features. Management guidelines suggest full body imaging at least every 2 years.
Treatment and interventions, such as surgery, are tailored to meet the needs of each patient with LDS. The frequency of medical appointments and need for surgical interventions will depend on the presence or absence of disease features and the severity of those features.[3][9]
Genetic Counselling
After a diagnosis, or suspected diagnosis of LDS is made, patients and their family members should see a genetic counsellor. A genetic counsellor can help educate patients about the disease characteristics and inheritance of LDS, and connect patients with support online or in their community. Genetic counsellors will spend time getting to know a patient and their family by taking a detailed family history. This allows genetic counsellors to asses which family members might also be at risk for LDS. Genetic counsellors are often responsible for explaining and arranging genetic testing. Many patients, upon hearing they have a genetic condition, are worried about children they already have or are planning to have. Genetic counsellors help guide patients through family planning and socials issues that may come up between family members, and arrange genetic testing for children that may have inherited LDS from their parent.
Pregnancy
As well as being counselled on the inheritance of LDS, women with LDS who are planning to have children will also be counselled on the risks during pregnancy. Severe complications of LDS in pregnant women have been reported and include aortic dissections and uterine rupture. These complications are life threatening for both the woman and her unborn child. Increased monitoring of cardiovascular symptoms are recommended for pregnant women. [9][10]
Psychosocial Issues
Many psychosocial issues can arise with LDS. The mean age of death in initial studies of LDS patients was 26.1 years. Although better surveillance and surgical treatments are presumed to increase life expectancy, patients with LDS are commonly afraid of the future and unpredictable nature of their condition. The burden of having a life-threatening genetic disorder that is often accompanied by differences in physical appearance can be especially heavy for adolescents as they begin to understand the significance of their diagnosis and as their social environment changes. The seriousness and hereditary nature of LDS means even a single diagnosis has the ability to affect relationships and communication within a family. Although these issues are introduced by the genetic counsellor, ongoing psychotherapeutic support may be needed for a patient or family.[3][9]
While the genetics team in key in making initial referrals to other doctors and clinics that will be apart of their patient's health care team, the responsibility of organizing and attending medical appointments falls to the patient. LDS patients are also required to limit their level of exercise and other activities that increase their heart rate. It is important to acknowledge the weight that these life-style restrictions can have on patients.[11]
Patient and Family Resources
References
- ↑ Loeys, B. L. et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat Genet 37, 275–281 (2005).
- ↑ Loeys, B. L. et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. The New England Journal of Medicine 355, 788–798 (2006).
- ↑ 3.0 3.1 3.2 3.3 MacCarrick, G. et al. Loeys–Dietz syndrome: a primer for diagnosis and management. Genet Med 16, 576–587 (2014).
- ↑ Boileau, C. et al. TGFB2 mutations cause familial thoracic aortic aneurysms and dissections associated with mild systemic features of Marfan syndrome. Nat Genet 44, 916–921 (2012).
- ↑ Lindsay, M. E. et al. Loss-of-function mutations in TGFB2 cause a syndromic presentation of thoracic aortic aneurysm. Nat Genet 44, 922–927 (2012).
- ↑ LWischmeijer, A. et al. Thoracic Aortic Aneurysm in Infancy in Aneurysms-Osteoarthritis Syndrome Due to a Novel SMAD3Mutation: Further Delineation of the Phenotype. Am. J. Med. Genet. 161, 1028–1035 (2013).
- ↑ Van Laer, L., Dietz, H. & Loeys, B. in Progress in Heritable Soft Connective Tissue Diseases (ed. Halper, J.) 802, 95–105 (Springer Netherlands, 2013).
- ↑ Azhar, M. et al. Transforming growth factor beta in cardiovascular development and function. Cytokine & Growth Factor Reviews 14, 391–407 (2003).
- ↑ 9.0 9.1 9.2 9.3 9.4 Loeys BL, Dietz HC. Loeys-Dietz Syndrome. 2008 Feb 28 [Updated 2013 Jul 11]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1133/
- ↑ Kunishige, H. et al. Surgical treatment for acute type A aortic dissection during pregnancy (16 weeks) with Loeys-Dietz syndrome. Gen Thorac Cardiovasc Surg 60, 764–767 (2012).
- ↑ Eton, D. T. et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas 3, 39–49 (2012).
See also
- Ehlers-Danlos syndrome Type IV (EDS-IV) and Marfan syndrome have overlapping characteristics to LDS, notably aortic aneurysms and dissections, and are often considered during the diagnosis process.