CourseCourse:MEDG550/Student Activities/EDS-IV
Overview
Ehlers-Danlos Syndrome (EDS) is a group of inherited disorders that affect the connective tissues of the body. Connective tissues support the skin, blood vessels, bones, and other organs and tissues. Vascular EDS (vEDS) was previously known as EDS type IV. The condition is characterized by severe arterial and digestive complications that are rarely observed in the other types. vEDS is rare, and is estimated to affect 1/50,000 to 1/200,000 individuals.[1]
What Does vEDS Look Like?

The common visible features of vEDS include easy bruising, thin and translucent skin with highly visible veins, hypermobility of the small joints (e.g. fingers and knuckles), and a characteristic facial appearance including thin lips, large prominent eyes, small chin, and thin nose.[2] The facial characteristics of vEDS are normal variations seen in everyday populations, however this specific combination of features are often observed in individuals with vEDS.
The other major features of vEDS are internal and often go unnoticed until there is a complication. These include:[2]
- Vascular complications
- Arterial aneurysm (enlargement of a blood vessel)
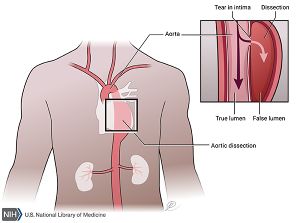
- Arterial dissection (a tear of the lining of an artery or blood vessel)
- Arterial rupture (breakage of an artery)
- Carotid cavernous sinus fistula (abnormal connection between the arteries and veins within the skull)
- Digestive complications
- Intestinal rupture (hole in the wall of the gastrointestinal tract)
- Pregnancy complications
- Uterine rupture (breach of the uterus)
The visible features of vEDS are relatively minor, so unless there is a family history of vEDS, it is usually not diagnosed until these vascular, digestive, or pregnancy problems arise.[2]
What Causes vEDS?
vEDS is a genetic disorder. All of the genetic information in our bodies can be thought of like an instruction book that provides a code for how our bodies grow, develop, and function. The genetic information is stored in smaller units of information known as genes, like pages in our instruction book. We have two copies of every gene, one from our mother and one from our father. Sometimes we have changes in our genes, like spelling mistakes on the pages of our instruction book, that effect the way the gene is able to function.
In vEDS, the majority of cases are caused by changes in the gene COL3A1. This gene provides instructions for making type III collagen. Collagens are a group of proteins, and are main component of connective tissue. Connective tissue supports skin, bones, tissues, and organs, and is essential for proper body structure and functioning. One of the collagens, type III collagen, is important for supporting the stretchable, hollow organs, like arteries, veins, the bowel, and the uterus. Another function of type III collagen is supporting the skin.[3] If there is a change in the gene COL3A1, type III collagen isn't properly made, and there is less support for blood vessels, internal organs, and skin. This is why people with vEDS may rupture arteries or organs, bruise easily, and have thin skin.
There are two general types of changes that cause vEDS. Most people with vEDS have changes in COL3A that affect the quality of the type III collagen protein[2] – the protein does not function in the way that it was intended to – this is the more classic, and most common, form of vEDS. More rarely, some people with vEDS have changes in COL3A1 that affect the quantity of type III collagen – the protein functions normally but not enough of it is made. People with vEDS caused by these changes typically have a less severe form of vEDS, and have may not have any complications until later into adulthood.[4] [5]
Rarely, cases of vEDS can be caused by changes in the gene COL1A1.[6] This gene provides instructions for making type I collagen. Changes in COL1A1 that cause vEDS similarly lead to fragility of the blood vessels and connective tissues.
How is vEDS Inherited?

vEDS is a genetic condition caused by gene changes in COL3A1 or COL1A1. The condition can be passed from parent to child. All cases are inherited in an autosomal dominant pattern. Everyone has two copies of every gene, and autosomal dominant inheritance means that only one copy of the gene needs to have a change to develop vEDS. The gene copy with the change is considered to be non-functional and dominant over the normal gene copy. Someone with vEDS has a 50% chance of passing on the non-functional copy, and a 50% chance of passing on the functional copy. This means that someone with vEDS has a 50% chance of having a child with vEDS, and a 50% chance of having a child without the condition.
About 50% of the time, this gene change is inherited from a parent, and 50% of the time the gene change is a new event[2] – the gene change did not come from a parent, and happened spontaneously during development. Even if the gene change is a new, spontaneous event, someone with vEDS now has the potential to pass vEDS down to their children.
How is vEDS Diagnosed?
Doctors diagnose people with vEDS by looking at their features and asking questions about their health. [2] For a doctor to diagnose someone with vEDS, the person needs to have at least 2 out of the 4 features listed below[6]:
- rip or hole in an artery
- hole in the intestines
- a rip in the uterus
- family members with vEDS
People with less severe features can also get diagnosed with vEDS. Usually genetic testing is needed to confirm the diagnosis in these cases. Some examples of minor features include [6]:
- skin that is thin and see-through
- distinct facial features such as thin lips and eyes that bulge
- fragile and thin skin on the hands and feet
- flexible joins (ex. fingers)
- bruising easily
As mentioned above, genetic testing is sometimes needed to confirm the diagnosis of vEDS[2]. Genetic testing looks to see if there is a change in the COL3A1 gene. Genetic testing is usually done by taking a person's blood. If no genetic change is found in the COL3A1 gene, then another test might be done to see if there is a change in the COL1A1 gene[6]. If a genetic change is still not found, this does not mean that the person does not have vEDS. Genetic testing is not perfect and some genetic changes may not be picked up by the test. In addition, scientists still do not know all of the genes that cause vEDS. Doctors might also take a piece of a person's skin to run a different type of test and take a closer look at the skin[2].
There are other medical disorders that look similar to vEDS. In children, the disorders that are most similar to vEDS are disorders that affect how the body makes blood clots. In adults, disorders that are similar to vEDS are other types of EDS. These are called Marfan Syndrome or Loeys-Deitz Syndrome[6]. Therefore, a doctor must consider all of these different disorders before making the diagnosis.
I Have Been Diagnosed With vEDS – What Happens Now?

After a diagnosis has been made (either clinically or using genetic or biochemical testing), cardiovascular surveillance is performed to identify developing aneurysms, dissections, or vascular ruptures – early identification and intervention can be life saving. People with vEDS should wear a MedicAlert® bracelet, and must seek immediate medical attention for sudden unexplained pain. Contact sports, heavy lifting, and weight-training should be avoided, but moderate recreational exercise is fine. Routine colonoscopy and elective surgeries should be avoided, and the costs and benefits of invasive medical procedures should be carefully weighed.[2] Certain medications should also be avoided, including aspirin, clopidogrel, and antivitamin K.[6]
Pregnancy is an especially high-risk time for women with vEDS. During pregnancy, women are at risk of uterine rupture and other organ and blood vessel ruptures. Pregnant women should be carefully followed by their medical team. Although this is a time of increased risk of serious complications, many women with vEDS have safe, successful pregnancies. [2]
Genetic Counselling
Genetic counselling is available to patients with vEDS, and to their family members. Genetic counsellors can help determine which family members may be at risk of carrying a COL3A1 or COL1A1 mutation, and facilitate genetic testing as necessary. Click here to find one near you.
Family Planning
Genetic counselling can also help couples understand their reproductive options. Prenatal diagnosis of vEDS may be of interest to some couples and is available when the family’s specific mutation has been identified with genetic testing.[2] Prenatal diagnosis requires invasive obstetric procedures, which increase the risk of complications for a pregnant woman with vEDS. Chorionic villus sampling can be done from 11 to 13 weeks gestation, and amniocentesis can be done after 15 weeks gestation. Preimplantation genetic diagnosis may also be of interest to some families when they have an identified genetic diagnosis. This allows for selection of embryos that do not carry the genetic change in order to have children unaffected by vEDS. Other options that may be of interest to couples include adoption, surrogacy, and egg/sperm donation.
Psychosocial Concerns
Genetic counsellors can also provide support to families surrounding the psychosocial concerns that may arise for individuals and families with vEDS. The condition is complex and often invisible, leading to misunderstanding among healthcare professionals, families, and society as a whole. Awareness of potential psychosocial concerns may be helpful for preparation and implementation of support systems. Everyone is unique and this list does not encompass all of the concerns that people may face.
- Individuals with vEDS [7] [8]
- Anxiety and depression
- Chronic pain from the condition itself and as a result of medical procedures
- Stigmatization based on altered body image from bruising, scarring, or mobility equipment
- Isolation from friends and family who may not understand the condition
- Life changes to manage symptoms can lead to grief over one's previous way of living
- Fear of arterial complications, getting worse, becoming unemployed, pregnancy, or getting skin ruptures
- Parents of children with vEDS [7] [8]
- With a new diagnosis, feelings of guilt, depression, shock, relief, or uncertainty are common
- Families with a previous child with vEDS may have already developed coping strategies
- Fear over their child having an arterial complication
- May be overprotective of affected children
- Stigmatization related to allegations of child abuse over easy bruisability
- Frustration with the medical system in not understanding the condition or being unable to find a diagnosis
Resources for vEDS Patients and Families
Ehlers Danlos National Foundation (US)
References
- ↑ [Steinmann, B., Royce, P. M., & Superti-Furga, A. (2002). The Ehlers-Danlos syndrome. Connective tissue and its heritable disorders, 431-524.],
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 [Pepin MG, Byers PH. Ehlers-Danlos Syndrome Type IV. 1999 Sep 2 [Updated 2011 May 3]. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2015. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1494/]
- ↑ [Abel, M. D., & Carrasco, L. R. (2006). Ehlers-Danlos syndrome: classifications, oral manifestations, and dental considerations. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 102(5), 582-590.]
- ↑ [Schwarze, U., Schievink, W. I., Petty, E., Jaff, M. R., Babovic-Vuksanovic, D. et al. (2001). Haploinsufficiency for one COL3A1 allele of type III procollagen results in a phenotype similar to the vascular form of Ehlers-Danlos syndrome, Ehlers-Danlos syndrome type IV. The American Journal of Human Genetics, 69(5), 989-1001.]
- ↑ [Leistritz, D. F., Pepin, M. G., Schwarze, U., & Byers, P. H. (2011). COL3A1 haploinsufficiency results in a variety of Ehlers-Danlos syndrome type IV with delayed onset of complications and longer life expectancy. Genetics in Medicine, 13(8), 717-722.]
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 [Malfait et al. (2017). The 2017 international classification of the Ehlers–Danlos syndromes. Am J Med Genet Part C Semin Med Genet 175C:8–26.]
- ↑ 7.0 7.1 [Giroux, C. M., Corkett, J. K., on, L. C. A.2016. The Academic and Psychosocial Impacts of Ehlers-Danlos Syndrome on Postsecondary Students: An Integrative Review of the Literature. ahead.org]
- ↑ 8.0 8.1 [Bulbena, A. et al. Psychiatric and psychological aspects in the Ehlers-Danlos syndromes. Am. J. Med. Genet. 175, 237–245 (2017).]