Course:MEDG550/Student Activities/Galloway-Mowat Syndrome
Overview
First described in 1968, Galloway-Mowat Syndrome (GAMOS) is a very rare condition caused by a genetic change; this condition often presents in individuals through many physical and developmental differences.[1] [2]
Prevalence
Statistics on the prevalence of Galloway-Mowat Syndrome in the world is limited. There likely exists between 54 and 70 reported cases of Galloway-Mowat Syndrome in the scientific literature, based on multiple sources.[2][3] Because cases can be mistakenly diagnosed as something else, or not diagnosed at all, it is difficult to have a true estimate of how many people have been affected.[2] There is also a lack of country-specific and worldwide statistics due to how rare the condition is. However, according to the NIH, there are fewer than 1000 people diagnosed with the condition in the USA. [4]
Symptoms

Galloway-Mowat is an extremely heterogenous condition, which means the type of symptoms of those with the condition may vary greatly from person to person, as well as the severity.[5] Symptoms typically involve neurological problems and early onset kidney disease, but can include many others listed below.[2][4][6]
*indicates the most common symptoms of Galloway-Mowat.
Neurological
Neurological symptoms describe abnormalities in the nervous system, particularly brain function and development in this case.
- Intellectual disability*
- Developmental delay*
- Fewer and more widely spaced ridges (gyri) in the brain
- Seizures
- Narrowing of the aqueduct of Sylvius (part of the brain that connects the third and fourth ventricles)
- Degeneration of the optic nerves (major nerve in the eyes) causing vision issues
Developmental delay can include the motor (movement) development of a child, language development, and emotional development. Because of this, most individuals with Galloway-Mowat are not able to sit on their own, perform controlled hand / limb movements, or communicate with others verbally.[2]
Renal

Renal symptoms describe abnormalities in kidney function.
- Nephrotic syndrome or kidney disease*
Nephrotic syndrome is commonly early onset, resistant to multiple medication treatments including steroids, and progresses to end-stage kidney disease very quickly.
Craniofacial
Craniofacial symptoms describe abnormalities in the development and overall structure of the head and/or face.
- Progressive microcephaly (decreased head size)*
- Underdevelopment of ear cartilage*
- Large ears
- Small lower jaw
- Dental abnormalities
- More closely or widely spaced eyes than normal
Musculoskeletal
Musculoskeletal symptoms describe abnormalities in the development and structure of bones and muscles in the body.
- Short height
- Vertebrae (bones in the spine) abnormalities
- Inward turned thumbs
- Bent fingers that cannot be flexed normally
- Increased or decreased muscle tone
- Mild or severe loss of strength of the limbs and sometimes face on one side of the body

Diagram of: A) Normal stomach B) Pre-stage hernia C) Milder stomach hernia D) Severe stomach hernia
Other
- Stomach hernia (portion of the stomach protrudes through the muscle wall)
- Immune system abnormalities
- Vision problems
- Congenital heart disease
- Hypothyroidism
Onset
The onset of symptoms varies between individuals with Galloway-Mowat Syndrome. Symptoms largely appear within the first few months of life, but can occur in the timeframe from birth to early childhood. There are also signs that can occur during pregnancy if the baby is affected by Galloway-Mowat, which includes reduced growth of the baby, microcephaly (small head), abnormal amniotic fluid level (too much or too little) and premature birth.[4][6]
Diagnosis
A diagnosis of Galloway-Mowat is commonly made after birth, through different tests, scans, and examinations. A physician will conduct a physical examination to identify any visible abnormalities in the head, face, and body. A CT scan, which scans the brain, may be ordered to provide the doctor with more information on internal brain abnormalities. A neurological examination can test the child's reflexes. Biochemical tests may be ordered to identify abnormal levels of the body's natural chemicals. A common example is testing for high protein in the urine (proteinuria), which is common in Galloway-Mowat Syndrome due to the kidney issues associated with this condition. Genetic testing can be done to identify if the child carries a harmful genetic change in a gene known to cause Galloway-Mowat Syndrome.[6][7]
Types of GAMOS
There are different types of Galloway-Mowat Syndrome depending on the gene that contains the harmful change; however, these known types do not include all known genes to be involved in this condition, as they are continuously being discovered. There are likely many unknown genes that may or may not fit into these types as well. Despite there being different types, each form of GAMOS is severe and have overlap in the common physical, neurological, and kidney-related symptoms.[3]
GAMOS1
Type 1 of this condition is caused by changes in the WDR73 gene. This is the second most type change to date, making up approximately 35.18% of reported families. The inheritance pattern is autosomal recessive (explained below).
GAMOS2
Type 2 of this condition is caused by changes in the LAGE3 gene. This is the fourth most common type to date, making up approximately 5.55% of reported families. The inheritance pattern is x-linked recessive (explained below).
GAMOS3
Type 3 of this condition is caused by changes in the OSGEP gene. This is the most common type to date, making up approximately 48.15% of reported families. The inheritance pattern is autosomal recessive.
GAMOS4
Type 4 of this condition is caused by changes in the TP53RK gene. This is the third most common type to date, making up approximately 7.40% of reported families. The inheritance pattern is autosomal recessive.
GAMOS5
Type 5 of this condition is caused by changes in the TPRKB gene. This is the least common type to date, making up approximately 3.70% of reported families. The inheritance pattern is autosomal recessive.
There is some available information on ethnic groups that are more commonly affected than others for GAMOS1, GAMOS3, and GAMOS4. Type 1 is most commonly seen in Amish families in North America and Arab families in Central Asia, West Asia, and North Africa. Type 3 is most commonly seen in Arab families, Caucasian families in North America, and families from Taiwan, Spain, and Pakistan. Type 4 is most commonly seen in South Korean families.[3]
Genetics
Inheritance Pattern: Autosomal Recessive (AR)

Galloway-Mowat Syndrome can be inherited in an autosomal recessive manner, depending on what genes are involved in causing the condition. This means that two copies of the mutated gene, or pathogenic variant, must be passed on, one from each parent, for the individual to be affected.
A pathogenic variant refers to a change in the DNA sequence of a gene that has harmful consequences to an individual's health. Autosomal refers to the genes that are on chromosomes other than the sex chromosomes. If someone only has one copy of a mutated gene known to cause Galloway-Mowat, they will be considered a carrier.[4]
If someone is a carrier, they typically do not exhibit any symptoms. If two parents are carriers of the mutation, there is a 25% chance of having a child with Galloway-Mowat, 25% chance of the child not inheriting either parent's Galloway-Mowat mutation, and 50% chance the child is a carrier like their parents.[4]
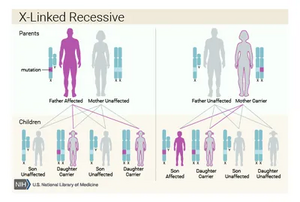
Inheritance Pattern: X-linked Recessive (XL)
Galloway-Mowat Syndrome can also be inherited in an X-linked recessive manner, depending on what genes are involved in causing the condition.
This form of the condition impacts males and females differently, because of the difference in sex chromosomes. Females typically have two X chromosomes, while males have one X and one Y chromosome. If a mutation in a gene on the X chromosome that causes Galloway-Mowat Syndrome is inherited by a a female, she may experience no symptoms or less severe symptoms because of the additional X chromosome. However, if a male inherits the affected X chromosome, there will likely be more severe symptoms, because he does not have another unaffected X chromosome.[4]
In a mother carrying the mutation for Galloway-Mowat, there is a 50% chance of it being passed down to her daughter's, who would be likely unaffected, while there is a 50% chance of passing it on to her sons, who would be affected more severely.[4]
Genes Involved
To date, the genes known to cause Galloway-Mowat Syndrome when there is a harmful change (pathogenic variant) include WDR4, NUP133, TPRKB, OSGEP, NUP107, WDR73, TP53RK, GON7, YRDC and LAGE3. All listed genes are inherited in an autosomal recessive manner as described above, except LAGE3, which is inherited in an x-linked recessive manner. There may be more genes involved in the condition that have not yet been discovered.[4][5][6][8]
Harmful changes in the gene OSGEP are most common and are associated with earlier onset kidney disease, while harmful changes in WDR73 is typically associated with later onset kidney disease.[6]
Genetic Counselling
Genetic counselling can assist patients and families with a diagnosis of Galloway-Mowat Syndrome through the following:
- Describing the genetic cause behind the condition (if known)
- Describing how the gene change responsible for the condition can be passed down through generations
- Providing reproductive counselling (risk of the condition recurring in future children based on family and medical history)
- Exploring management options
- Describing and Coordinating genetic testing to confirm a diagnosis
- Identifying and providing patient resources
- Providing psychosocial support
- Facilitate decision-making regarding management and/or testing options
Treatment and Management
To date, there has been no effective and specific treatment for Galloway-Mowat Syndrome. Treatments therefore focus on the specific symptoms present, such as kidney issues and seizures, which can be different depending on the person. Kidney issues can be treated with dialysis (process of removing toxins from the blood), and/or medications. Symptoms like seizures can also possibly be treated with medications. Prognosis is poor and most children with this condition pass away in early childhood. Although most reported cases involve children passing away within the first few months to first few years of life, there can be variation in life expectancy depending on which gene is affected (what type of GAMOS a child has). There have been reports of individuals passing away at later ages, including age 8, 17, and 28. However, these individuals experienced later onset kidney disease, which rapidly progresses from diagnosis and is the most common direct cause of death in patients with this condition.[6][3][8]
Psychosocial Components
Galloway-Mowat Syndrome is a genetic condition, meaning it is caused by harmful changes in the DNA that can occur at random. Some families may feel guilty for passing on a genetic change that causes this condition. It is important to note that it is no one's fault, and there is no control over if the genetic changed is passed on from parent to child. As previously mentioned, genetic counselling can help families address this, along with other difficult emotions that may follow this diagnosis.
Resources
- GARD - Genetic and Rare Disease Information Center
- NORD - National Organization for Rare Disorders
- National Kidney Foundation
- Kidney Foundation of Canada
References
- ↑ Galloway,, W.H.; Mowat (A.P.). "Congenital Microcephaly with Hiatus Hernia and Nephrotic Syndrome in Two Sibs" (PDF). Journal of Medical Genetics. 5: 319–321 – via NIH. line feed character in
|title=at position 47 (help); Check date values in:|date=(help)CS1 maint: extra punctuation (link) - ↑ 2.0 2.1 2.2 2.3 2.4 "Galloway-Mowat Syndrome". National Organization for Rare Disorders. May 9, 2016. Retrieved January 12, 2024.
- ↑ 3.0 3.1 3.2 3.3 Chen, Yan; Yang, Yan; Rao, Jia; Bai, Haitao (February 8, 2023). "Diagnosis delay a family of Galloway-Mowat Syndrome caused by a classical splicing mutation of Lage3". BMC Nephrology. 24: 29 – via BMC Nephrology.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 "Galloway-Mowat Syndrome". Genetic and Rare Diseases Information Center. November 2023. Retrieved January 13, 2024.
- ↑ 5.0 5.1 Rosti, Rasim O.; Dikoglu, Esra; Zaki, Maha S.; Abdel-Salam, Ghada; Makhseed, Nawal; Sese, Jordan C.; Musaev, Damir; Rosti, Basak; Harbert, Mary J. (January 5, 2016). "Extending the Mutation Spectrum for Galloway–Mowat Syndrome to Include Homozygous Missense Mutations in theWDR73 Gene". American Journal of Medical Genetics. 170: 992–998 – via Wiley Online Library.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 "Galloway-Mowat Syndrome". Orphanet. May 2020. Retrieved January 14, 2024.
- ↑ Akhtar, Naureen; Kiran, Sadia; Hafeez, Farkhanda (July 30, 2008). "Galloway-Mowat Syndrome" (PDF). Journal of the College of Physicians and Surgeons Pakistan. 18: 520–521 – via World Health Organization (WHO).
- ↑ 8.0 8.1 "GALLOWAY-MOWAT SYNDROME 1; GAMOS1". OMIM. October 24, 2021. Retrieved January 14, 2024.