Course:RSOT513/2010W2/ortho/ Carpal Tunnel Syndrome
Introduction
Carpal tunnel syndrome (CTS) is a collection of symptoms that develop as a result of compression of the median nerve as it passes through the carpal tunnel. The carpal tunnel is a passage created by the carpal bones which form an arch, and a fibrous band of tissue called the flexor retinaculum. The pisiform and hammate bones are situated on the ulnar side, the scaphoid and trapezium are on the radial side, and the flexor retinaculum covers the ventral surface.[1]
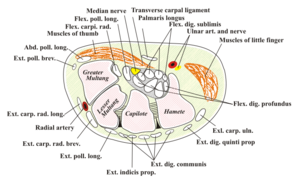
There are a number of soft tissue structures that pass through the carpal tunnel including the long flexor tendons of the fingers and thumb, numerous blood vessels, and the median nerve. The median nerve supplies sensory innervation to digits 1,2 and 3, as well as the medial aspect of digit 4. It also provides motor innervation to the muscles of the thenar eminence.[1]
Etiology
Median nerve entrapment is caused by increased pressure within the carpal tunnel. The increased pressure can be caused by a decrease in the carpal tunnel’s size, or an increase in the volume of contents that pass through the tunnel as with inflammation.[1]
The decrease in the size of the carpal tunnel may result from various mechanisms including wrist trauma of the bony tissue or congenital reduction in the carpal tunnel’s size and shape.[2]
An increase in the volume of contents that pass through the tunnel may result from repetitive compression due to posture or perpetual muscle contractions. Tension overload and repetitive motions at the wrist expose tissues to frictional forces that can lead to microtrauma. This results in inflammation of the tendon sheath (tenosynovitis), edema, and scar tissue formation. The result is increased pressure in the carpal tunnel and compression of the median nerve.[2] Overall fluid retention during pregnancy can also lead to CTS by increasing tissue volume at the wrist.[2]
Although there are many factors that can increase the risk of CTS, such as those listed above, in some cases the specific cause for the individual is idiopathic.[2] However, CTS can also have systemic causes including diabetes mellitus, rheumatoid arthritis, and hypothyroidism. It can occur in isolation or be associated with other pathologies such as De Quervain Syndrome, trigger finger, epicondylitis or shoulder pathologies.[2]
Prevalence
The estimated prevalence rate of Carpal Tunnel Syndrome (CTS) in the general population varies, depending on how the syndrome is defined and diagnosed.[3] The prevalence rate of CTS symptoms in the general population has been reported at 14.4%, while the prevalence of CTS as confirmed by clinical examination is 3.8% and shrinks to 2.7% when confirmed by both clinical examination and nerve conduction test.[4] So although symptoms of tingling, numbness and pain in the hands are common in the general population, only 1 in 5 people with symptoms are likely to have a confirmed diagnosis.
CTS is more common in women than men ([2],[4],[5]) and most often develops in individuals between the ages of 40-50.[2] Prevalence is also higher among pregnant women, although there is limited information regarding the exact incidence.[1] In most cases, symptoms resolve after childbirth, although mild symptoms may still exist after three years in approximately half of these women.[6]
Common Signs and Symptoms
General Criteria
- Pain, or paraesthesia, or sensory loss in the median nerve and one of the following:
- Tinel’s sign positive
- Nocturnal exacerbation of symptoms
- Motor loss with wasting of abductor pollicis brevis
- Abnormal nerve conduction time[2]
Characteristics
- CTS is characterised by tingling, pins and needles, numbness, pain or burning sensations in the areas of median nerve distribution, which includes digits 1 to 3.5 and the lateral 2/3 of the palm.
- Pain may be reported as a dull aching discomfort in the hand or forearm.
- Pain may often be reported as being worse at night and it may cause waking.
- It may be in one or both hands, although it is common for the dominant hand to be affected more frequently.
- Symptoms can worsen during sleep, sustained hand or arm positions, or repetitive actions of the hand or wrist. *Symptoms may be improved by changing hand position.[7]
Physical Appearance
- Affected hand may appear normal on physical examination although there is sensory loss.[7]
- Swelling or changes in skin colour may occur on affected hand.
- Dry skin may be present on the thumb, index and middle fingers.
- Atrophy of thenar eminence may be evident but is a late sign and indicative of significant functional loss.[2]
Function
CTS may cause an individual to have:
- Difficulty with tasks requiring precise and forceful finger movements (ie. buttoning shirt, tying shoes, unlocking a door)
- Weak grip, which may cause the individual to drop things
- Weakness, particularly of the thumb
- Clumsiness of fine finger movements or reduced manual dexterity[7]
Differential Diagnoses
There are numerous differential diagnoses that should be ruled out when making a diagnosis of CTS. These include cervical radiculopathy at C6/7, generalized peripheral neuropathies or ulnar neuropathies, neurologic conditions such as multiple sclerosis, vascular conditions such as Raynaud’s phenomenon, and osteoarthritis.[7]
Implications of CTS on Occupation
Self-Care
Performance of regular daily activities can be difficult for people with CTS. Because pain is often worse at night, and because many people sleep in a fixed arm position, people with CTS may have difficulty sleeping or wake throughout the night.[8] Other self care activities that require “precise and forceful finger movements” [7] like tying shoes, fastening buttons or zippers, applying makeup and brushing teeth, may be difficult. To further illustrate this, Bylund & Ahlgren interviewed eight women who worked with vibrating tools and who reported CTS.[8] These women reported difficulty with dressing, taking off rings, brushing their hair and teeth, and holding a fork and knife.
Productivity
Numerous studies ([9],[8],[10],[11]) indicate that work that includes repetitive movements at the wrist and hands can be risk factors for CTS. Additionally, once CTS is developed, these work activities are often difficult to perform and the productive occupation may be stopped altogether.
One study investigating work-related and non-work-related risk factors of CTS found force exertion of over 1 kg, bending/twisting of the wrists, rapid movement of the hands (as in assembly line work) and using vibrating tools to be risk factors for developing CTS. In correlation with these findings, studies investigating industries and occupations with reported cases of CTS found jobs involving the previous tasks and movements as high risk. The most cases of CTS were reported with cooks followed by gardeners, plumbers, bricklayers and those with construction jobs. For women, high risk jobs included cleaning, dental hygiene, clerical work, public services and trades.[11] Bylund & Ahlgren found that women with carpal tunnel syndrome experienced difficulty completing basic household chores like vacuuming, cleaning windows, peeling potatoes, carrying grocery bags, ironing, and hanging up laundry and curtains.[8] These women also reported difficulty holding a pen and writing for an extended period of time. Clients who develop CTS and are employed in these high risk industries will experience disruption in their productive occupations due to the strain involved in the motions and tasks of their work.
Leisure
One qualitative study [12] on adaption to CTS found participants were in denial of their symptoms and did not seek treatment for an average of 20.4 months. The five participants had similar experiences of attributing their symptoms to either work or wrist positioning and did not seek treatment until it was a last resort due to negative life changing adaptations. Participants reported giving up valued leisure occupations such as gardening, baking, knitting, and sewing. They also reported wearing less make-up, resting poorly and avoiding painful tasks at work which are further examples of how CTS affected their daily occupations.[9]
Role of Occupational Therapy
Assessment
Tinel’s sign and Phalen’s tests can be used to assess for CTS. They may be administered by an occupational therapist (OT). Tinel’s sign involves tapping at the volar wrist while Phalen’s test involves maintaining wrist flexion for 60 seconds. In both tests, a positive sign is indicated by numbness, tingling or pain in the thumb, index and half of the middle finger. Following positive signs, the OT may perform manual muscle testing for grip and pinch strength and assess range of motion.[13] The OT may perform a detailed step-by-step breakdown of what's involved in the activity to look at the specific tasks that could be affected by or be contributing to CTS symptoms. For example, the OT may analyze the activity of cooking. The OT may find, for example, that repetitive lifting of heavy skillets is a contributing factor to the individual’s CTS symptoms. The OT may also observe the environment in which the activity is being performed and identify risk factors and compensatory strategies.[13]
Intervention
OTs provide protective and corrective non-surgical measures for CTS and focus intervention on the person's physical abilities, environment, and the activities they engage in. OT intervention has an emphasis on enabling function in self-care activities, leisure and paid or unpaid work. At the level of person, occupational therapists can provide education and/or direct intervention for physical symptom treatment and management. At the levels of environment and occupation, OTs provide education and modifications related to the method of task completion, including equipment and tools used, and the setting in which it is being performed. OTs who provide intervention for individuals with CTS may also be hand therapists. Bash & Farber state that to become a hand therapist, an individual must be a physical or occupational therapist with at least 5 years experience, including 2000 hours of therapy pertaining directly to hands, and a certification exam is required.[14]
Education
OTs play a large role as educators. Education may be provided to an individual client or a group of people. Individuals with CTS or at risk for CTS may benefit from education in the areas outlined below:
- signs & symptoms of CTS
- options for treatment: surgical and/or non surgical interventions
- how to reduce risks & decrease symptoms of CTS
- splint wearing regimen
- body mechanics & exercises
- task adaptation
- adaptive tools
- workplace adaptations
Physical Symptom Management Techniques
Splinting
OTs often use wrist splinting as a form of treatment. Splints may be pre-fabricated or customt-fit. Prefabricated splints are sold in health care supply stores and are an inexpensive option for clients. Prefabricated splints may be used but the fit may not be precise enough for all individuals. In this case, a custom fit splint is required.[15] A OT will fabricate a custom-fit splint by molding thermoplastic material unique to the client's hand, wrist and forearm. Splints can be based on the front (palmar), back (dorsal) or outer side (pinky) of the arm. According to Muller et al’s systematic review on interventions for CTS, volar cock-up splints and ulnar gutter splints are similar in their improvement of symptoms and function.[16] Dorsal splints are also recommended for CTS as they reduce pressure placed on the volar wrist.[17] Splints aim to immobilize the wrist to decrease pressure in the carpal tunnel.[1] Restricting wrist motion eliminates the repetitive movement and tension overload in the carpal tunnel.[2] This gives the tendon sheaths a chance to heal, reducing swelling, which then may decrease the pressure on the median nerve.[2] Splints also aim to keep the wrist at a certain angle to decrease pressure within the carpal tunnel.[17] Although there has been debate about the best angle for wrist immobilization, [18] the authors of a systematic review on non surgical carpal tunnel treatments conclude that “there is limited evidence that the use of a wrist splint in neutral position is more effective than an extended wrist position of 20 degrees in patients with CTS in the short term.”([19], p983) In another systematic review on interventions for CTS, Muller et al found that wearing a nocturnal splint as well as wearing a splint during aggravating activities alleviate symptoms of CTS (numbness, pain and tingling) better than no treatment.[16] It follows that decreasing symptoms of CTS improves overall occupational function in activity.[20]
Other
An occupational or physiotherapist working as a hand therapist may be involved in other areas of treatment for the symptoms of CTS depending on their scope of practice.[16] These treatments may include but are not limited to ultrasound, electromagnetic field therapy, magnetic therapy, low level-laser therapy, or nerve gliding exercises.([16],[19])
Modifications for Prevention/Reduction of Symptoms
Modification of Occupation (Task)
Modification of a task is about adjusting behaviors and actions that may contribute to the development or exacerbation of CTS. As part of the assessment, the OT will conduct an activity analysis to identify areas where change may be needed. Once a task is analyzed, alternative methods can be negotiated or discussed with the client. As Doheny et al suggest, tasks can be redesigned to include diversity and thus limit repetitive movements that can aggravate CTS.[21] For example, Keir et al suggest breaking up the repetitive action of using a computer mouse with other tasks because mouse use was shown to increase carpal tunnel pressure. This study also suggests minimizing wrist extension through appropriate body posture at the workstation which may help to reduce carpal tunnel pressure.[22] A review of the literature has found evidence supporting the use of exercise and/or rest breaks in reducing musculoskeletal discomfort during computer work.[23] Faucett et al found that people with CTS were more likely to continue with their current jobs if modifications were made to the tasks. Two of these modifications included limiting repetitive tasks and decreasing work time.[24] OT's can provide recommendations on job modifications to reduce risk factors by modifying client's work tasks.
Modification of Equipment and Tools
A major role of OTs is to introduce modified equipment and adaptive aids to enable occupational performance despite physical limitations. Modifying equipment and tools can correct positioning of the hand (e.g. keep it in a more neutral position) and reduce the hand force required to complete an action. For example, Dolby Laboratories introduced hand tools that reduced the hand force required, distributed the force over a larger surface area of the hand, and corrected the positioning of the hand through specially shaped handles that did not impinge on the median nerve area of the palm. These tools were designed to reduce risk factors associated with cumulative trauma disorders such as CTS.[25] For example, specialized spring-loaded pliers reduced the force required to cut wire for electronic assembly purposes. Adaptive aids can be useful in enabling individuals with CTS to participate in their chosen activities. One such adaptation is increasing the diameter of handles so that less grip strength is needed to grasp an object.[26] Any handle can be built up in this way. For example, someone who has CTS may have difficulty holding their toothbrush or utensils while eating. OTs can easily adapt these tools or purchase already adapted tools for a client. Specific risk factors that can contribute to CTS such as vibration can be reduced by introducing new tools with lower vibration levels as well as anti-vibration gloves.[27]
Modification of Environment
Another important avenue of occupational therapy is adapting the environment to facilitate occupational performance of a particular task. When modifying an environment, often the equipment and tool adaptations are part of that environmental change. In the management of CTS, workstation modification (i.e. adapting the work environment) is a large part of OT intervention. By adjusting the workstation equipment, such as desks, chairs, monitors, and keyboards, the ideal position of the wrist and forearm can be achieved. This can help alleviate symptoms of CTS as well as prevent further damage and strain.[21] For example, there is moderate evidence that a modified ergonomic keyboard is more effective than a regular keyboard at relieving symptoms of CTS.[19] The addition of forearm supports can help to facilitate appropriate posture of the wrist by preventing extension while using a mouse.[22] Attention should also be given to psychosocial aspects of a work environment, such as job demands and job control, as they may help or hinder return to work and level of functioning within the workplace for those individuals with CTS.[28] Similar to the work environment, OTs can help adapt the home environment through the introduction of adaptive aids and adjustment of furniture or equipment. The interventions for CTS mentioned above can be used together as illustrated in a study by Bash and Farber. These authors found that many hand therapists with symptoms of CTS not only wore splints, but also engaged in modifying their tasks, tools and environments as part of their own intervention plan.[14] Hand therapists are an example of a population that has been found to have high instances of CTS due to repetitive, stressful movements on the job. The hand therapists in this study used the following intervention strategies and reported symptom relief:
- made ergonomic changes to the work station (modify environment)
- used adaptive scissors and shears (modify tools/equipment)
- reheated splint material to trim edges (modify task)
- changed hand position (modify task)
- used assistive equipment for scar massage (modify tools/equipment)[14]
Summary
In summary, OTs are involved in the assessment and intervention process with clients with CTS. Within the area of intervention, OTs provide education; symptom management techniques such as splinting; and modification of specific tasks, equipment and the environment.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Walker JA. Management of patients with carpal tunnel syndrome. Nursing Standard. 2010. 24(19): 44-48. Cite error: Invalid
<ref>tag; name "Walker" defined multiple times with different content - ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Luchetti R, Amadio, P, editors. Carpal tunnel syndrome. Berlin; New York: Springer; 2006.
- ↑ Descatha A, Dale AM, Franzblau A, Coomes J, Evanoff, B. Comparison of research case definitions for carpal tunnel syndrome. Scand J Work, Environ Health. Forthcoming 2011.
- ↑ 4.0 4.1 Bland, JD. Carpal tunnel syndrome. British Medical Journal. 2007. 335(7615):343-46.
- ↑ Bland JD, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom. J Neurol Neurosurg Psychiatry.2003;74:1674–79.
- ↑ Mondelli M, Rossi S, Monti E, Aprile I, Caliandro P, Pazzaglia C, Romano C, Padua L. Long term follow-up of carpal tunnel syndrome during pregnancy: a cohort study and review of the literature. Electromyogr Clin Neurophysiol. 2007 Sep;47(6):259-71.
- ↑ 7.0 7.1 7.2 7.3 7.4 NHS Clinical Knowledge Summaries. Carpal Tunnel Syndrome [Internet]. 2008 [updated 2008 Oct; cited 2011 Mar 24]. Available from: www.cks.nhs.uk/carpal_tunnel_syndrome
- ↑ 8.0 8.1 8.2 8.3 Bylund S, Ahlgren C. Experiences and consequences for women withhand-arm vibration injuries. Work. 2010;35(4): 431-439.
- ↑ 9.0 9.1 Palmer K, Harris E, Coggon D. Carpal tunnel syndrome and its relation to occupation: a systematic literature review. Occupational Medicine. 2007 Jan; 57(1): 57-66.
- ↑ Maghsoudipour M, Moghimi S, Dehghaan F, Rahimpanah A. Association of occupational and non-occupational risk factors with the prevalence of work related carpal tunnel syndrome. J Occup Rehabil. 2008 Apr 17;18:152–156.
- ↑ 11.0 11.1 Roquelaure Y, Ha C, Nicolas G, Pelier-Cady MC, Mariot C, et. al. Attributable risk of carpal tunnel syndrome according to industry and occupation in a general population. Arthritis Rheum. 2008 Sept 15;59(9):1341-1348.
- ↑ Hope M. Patients’ health beliefs and adaptation to carpal tunnel syndrome based on duration of symptomatic presentation. J Hand Ther. 2007;20(1):29–36.
- ↑ 13.0 13.1 Cooper C. Hand impairments. In: Radomski MV, Trombly Latham CA, editors. Occupational therapy for physical dysfunction. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2008.
- ↑ 14.0 14.1 14.2 Bash DS, Farber RS. An examination of self-reported carpal tunnel syndrome symptoms in hand therapists, protective and corrective measures and job satisfaction.Work.1999;13:75-82.
- ↑ Robert C. Byrd Health Sciences Center Department of Occupational Therapy. Carpal tunnel syndrome [Internet]. 2011. Available from http://www.hsc.wvu.edu/som/ot/Education/OT-Connect/Limitations-and-Impairments/Carpal-Tunnel-Syndrome/Default.aspx
- ↑ 16.0 16.1 16.2 16.3 Muller M, Tsui D, Schnurr R, Viddulph-Deisroth L, Hard J. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:210-228. doi: 10.1197/j.jht.2004.02.009.
- ↑ 17.0 17.1 Deshaies LD. Upper extremity orthoses. In: Radomski MV, Trombly Latham CA, editors. Occupational therapy for physical dysfunction. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2008.
- ↑ Burke DT, Burke MM, Stewart GW, Camber A. Splinting for carpal tunnel syndrome: in search of the optimal angle. Arch Phys Med Rehabil. 1994 Nov;75(11):1241-1244.
- ↑ 19.0 19.1 19.2 Huisstede BM, Hoogvliet P, Randsdorp MS, Flerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. part I: effectiveness of nonsurgical treatments- a systematic review. Arch Phys Med Rehabil. 2010;91:981-1004. doi:10.1016/j.apmr.2010.03.022.
- ↑ Corbin DE. Carpal tunnel syndrome recovery. Occup Health Saf. 2000 Apr;69(4):84-86.
- ↑ 21.0 21.1 Doheny M, Linden P, Sediak, C. Reducing orthopaedic hazards of the computer work environment. Orthop nurs. 1995 Jan;14(1):7-15.
- ↑ 22.0 22.1 Keir PJ, Bach JM, Rempel, D. Effects of computer mouse design and task on carpal tunnel pressure. Ergonomics. 1999;42(10):1350-1360.
- ↑ De Vera Barredo R., M. The effects of exercise and rest breaks on musculoskeletal discomfort during computer tasks: an evidence-based perspective. 2007. J. Phys. Ther. Sci. 19:151-163.
- ↑ Faucett J, Blanc PD, Yelin E. The impact of carpal tunnel syndrome on work status: implications of job characteristics for staying on the job. J Occup Rehabil. 2000;10(1):55-69.
- ↑ Weigel M. Case study ergonomic tools: beefing up the toolbox. Occup Health Saf. 1999 Jul;68(7):71-2 .
- ↑ Trombly Latham CA. Occupation as therapy: selection, gradation, analysis, and adaptation. In: Radomski MV, Trombly Latham CA, editors. Occupational therapy for physical dysfunction. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2008.
- ↑ Jetzer T, Haydon P, Reynolds D. Effective intervention with ergonomics, antivibration gloves, and medical surveillance to minimize hand-arm vibration hazards in the workplace. J Occup Environ Med. 2003;45:1312-1317. doi: 10.1097/01.Jo.0000099981.80004.c9.
- ↑ Ginemo D, Amick III BC, Habeck RV, Ossmann J, Katz JN. The role of job strain on return to work after carpal tunnel surgery. Occup Environ Med. 2005;62:778-785. doi:10.1136/oem2004.016931.