Course:PostgradFamilyPractice/ExamPrep/99 Priority Topics/Lacerations
Lacerations - Key Features
1. When managing a laceration, identify those that are more complicated and may require special skills for repair (e.g., a second- versus third-degree perineal tear, lip or eyelid lacerations involving margins, arterial lacerations).
2. When managing a laceration, look for complications (e.g., flexor tendon lacerations, open fractures, bites to hands or face, neurovascular injury, foreign bodies) requiring more than simple suturing.
3. Given a deep or contaminated laceration, thoroughly clean with copious irrigation and debride when appropriate, before closing.
4. Identify wounds at high risk of infection (e.g., puncture wounds, some bites, some contaminated wounds), and do not close them.
Generally, do not close:
• Crush injuries
• Puncture wounds
• Bites involving the hands and feet
• Wounds more than 12 hours old (24 hours old on face)
• Cat or human bites, except those to the face
• Bite wounds in compromised hosts (eg, immunocompromised, absent spleen or splenic dysfunction, venous stasis, diabetes mellitus [adults])
Similarly, consider antibiotic prophylaxis in the following cases:
• Animal bite wounds at high risk for infection
• Deep puncture wounds, especially cat bites
• Moderate to severe wounds with associated crush injury
• Wounds in areas of underlying venous and/or lymphatic compromise
• Wounds on the hand(s) or in close proximity to a bone or joint
• Wounds requiring surgical repair
• Wounds in immunocompromised hosts
5. When repairing lacerations in children, ensure appropriate analgesia (e.g., topical anesthesia) and/or sedation (e.g., procedural sedation) to avoid physical restraints.
6. When repairing a laceration, allow for and take adequate time to use techniques that will achieve good cosmetic results (e.g., layer closure, revision if necessary, use of regional rather than local anesthesia).
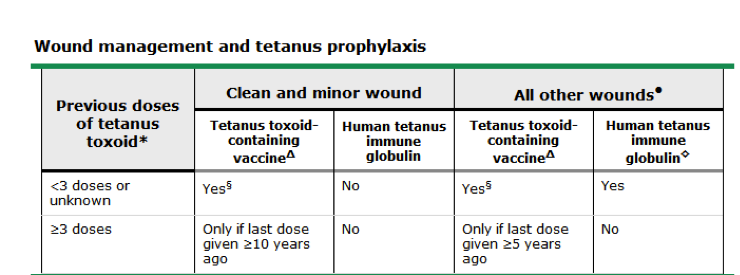
7. In treating a patient with a laceration:
a) Ask about immunization status for tetanus.
b) Immunize the patient appropriately.
Source: Up to date