Course:MEDG550/Student Activities/X-linked Retinoschisis

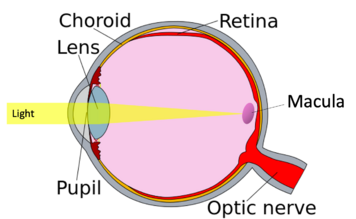
X-linked retinoschisis (also known as X-linked congenital retinoschisis or XLRS), is a genetic condition that causes impaired vision, and only affects males most of the time. Decline in vision usually happens early in life and is generally stable until a person is in their 50s or 60s. It is caused by a genetic change in the RS1 gene that affects the production of an important protein found in the retina, retinoschisin[1][2][3]. The retina is a thin layer of tissue on the inside back wall of the eye made up of millions of light-sensitive cells that sends visual information to the brain[4].
What causes X-linked retinoschisis?
X-linked retinoschisis is a genetic condition caused by variants (spelling changes) on the RS1 gene. This gene, which is found on the X chromosome, is responsible for the production of the retinoschisin protein[1][2]. Spelling changes in this gene can cause not enough retinoschisin to be made, no retinoschisin to be made, or the production of retinoschisin that does not work well.
Retinoschisin is an important protein found in the retina[1], the layer of cells in on the inside back wall of the eye that allows individuals to see[4]. Retinoschisin is responsible for holding cells together, and when it is no longer working. cells separate from one another and cause tears in the retina. When these tears form, the cells that make up the retina start to die, which together lead to a decline in vision[3].
What are the symptoms of X-linked retinoschisis?
The symptoms of XLRS are very variable – ranging from mild to severe, even in individuals with the same genetic variant[1]. This condition mostly affects males, but some females have been found to have very mild symptoms.
Impaired Vision
Individuals affected with XRLS will have a decline in vision within their first decade of life, generally by early elementary school[3][5]. Within the first and second decade of life, vision may continue to decline but will then stabilize until the individual is in their 50s or 60s. Color vision is normal most of the time[5].
Specifically, the tears in the retina decrease the sharpness of vision in both eyes[3][5]. Most of the time, tears are found in the area of the retina called the macula, which is responsible for sharp vision in the center of the visual field, causing reduced sharpness in central vision. This will result in difficulty in some everyday activities that require attention to detail like reading, recognizing faces and driving[1]. Occasionally, side vision is affected due to tears in other areas of the retina. This reduction in vision is not correctable by glasses or contact lenses[3][5].
In their 50s and 60s, individuals affected by XLRS may see further decline in vision that may progress to blindness[3][5].
Other Symptoms
Some other symptoms can include[3][5]
- Cystic macular lesions (blisters) in the retina which can worsen vision loss
- Retinal detachment (retina being pulled from it’s normal position)
- Leakage of blood vessels in the retina due to tears close to the vessels (vitreous hemorrhage)
- Involuntary movement of the eyes
- Eyes that do not appear to be looking in the same direction
- Farsightedness
- Flecks/dark spots on the retina
How is X-linked retinoschisis diagnosed?
Because symptoms of X-linked retinoschisis usually appear in the first decade of an individual’s life, it is usually diagnosed when they start school due to low vision and difficulty with reading[1][6]. There are certain findings that are suggestive of a diagnosis of XLRS. An ophthalmologist (eye doctor) will be able to diagnose XLRS if some of the following features are present in an individual:
- Reduced sharpness of vison in both eyes
- No complaint of difficulty to see in dim lighting (as compared to vision in regular lighting)
- Tears in the retina in the shape of a spoke wheel seen on an eye exam in both eyes
- Suggestive results in the following tests:
- Spectral domain optical coherence tomography (SD-OCT)
- Electroretinogram (ERG)
Genetic testing can also diagnose XLRS if a spelling change in the RS1 gene is found[1][6]. A family history of XLRS can also help with the diagnosis process.
How is X-linked retinoschisis treated?
Management
Though there is currently no cure for XLRS, it is possible to manage the symptoms that an individual has in the following ways:
- Low-vision services
- To optimize vision that is remaining, certain services are available to people with low vision. These services may vary based on the age of the individual[1][6].
- Children with XLRS would qualify for an individualized education plan which can be provided by their school.
- Obtaining a restricted driving license is possible for some individuals.
- Medication
Surgery
In the case of complications such as retinal detachment and vitreous hemorrhage surgeries such as vitrectomy or scleral buckling are offered[6].
Surveillance
Close follow up is the best tool for surveillance of XLRS symptoms and their progression[1]. It is recommended that children younger than ten-years-old receive annual evaluations by an ophthalmologist. Older children and adults can have less frequent follow-up as they are more likely to be able to detect changes in their vision.
Lifestyle Changes
It is recommended to avoid high contact sports or any other activities that may cause head trauma to avoid retinal detachment or vitreous hemorrhage[1].
Therapies
There are currently no therapies available to treat all of the symptoms of XLRS[1]. There are however ongoing clinical trials. To look into the option of joining these or any new clinical trials and for more information, click here. A primary care professional, ophthalmologist or genetic counsellor can help individuals with decisions regarding clinical trials.
How many people have X-linked Retinoschisis?
X-linked retinoschisis is found in about 1 in 5,000 to 1 in 25,000 people[1].
Genetic Counselling
For those with a family history or those living with XLRS, genetic counselling can provide several benefits. A genetic counsellor can explain the cause, the symptoms of the condition, as well as facilitate diagnostic and genetic testing. A genetic counsellor can also discuss the emotional and social impact that XLRS can have on families.

How is X-linked Retinoschisis passed down in my family?
X-linked Retinoschisis is an X-linked recessive condition[1]. Due to the way that it is inherited, XLRS affects more males than females. This is because the RS1 gene is on the X chromosome. Females have two X chromosomes (one inherited from their mother and the other from their father). Thus, even if one copy has the spelling change, the other can still produce retinoschisin. Females with one affected copy of the RS1 gene and one normal copy of the RS1 gene are called carriers. Males on the other hand, only have one X chromosome (and a Y chromosome) and therefore if their only X chromosome has a RS1 variant they will be affected.
The children of females who are carriers of XLRS have a 50% chance of inheriting the altered gene from their mothers[1]. Sons of a male with XLRS will not be affected as they will only be inheriting their father’s Y chromosome. Daughters of a male with XLRS will be carriers.
Although XLRS generally runs in a family, it is possible for a family with no history of the condition to suddenly have a son with the disease[1]. This can be caused by a de novo (new) spelling change that occurred in only the individual with XLRS. It can also be due to the spelling change only being passed down through females of the family.
How then might a diagnosis of X-linked retinoschisis affect my family?
Family members of individuals that have X-linked retinoschisis may be wondering how the diagnosis in their family might be affecting them.
Carrier Screening
Carrier screening is used to determine if someone is a carrier of XLRS[1]. This would only happen in females as any males that have the affected RS1 gene will have XLRS. If a female is found to have one copy of the affected RS1 gene, this can inform their future family planning. It can also inform the need for more routine follow-up with an ophthalmologist (due to the low chance that they may develop symptoms)[1][6]. Carrier screening may be offered to sisters and mothers of males diagnosed with XLRS.

Family Planning
The children of females who are carriers of XLRS have a 50% chance of inheriting the altered gene from their mothers[1]. Sons of a male with XLRS will not be affected as they will only be inheriting their father’s Y chromosome. Daughters of a male with XLRS will be carriers. Talking to a genetic counsellor would also be a good resource.
Prenatal Testing and Preimplantation Genetic Testing are available for families that have a chance of having a child born with XLRS[9]:
- Prenatal Testing: This involves testing the RS1 gene of a baby during pregnancy to see if it has a spelling change. Two options currently exist for this type of testing:
- Amniocentesis: Typically done after 15 weeks of pregnancy, this procedure involves inserting a needle through the abdomen of the mother to collect amniotic fluid from around the baby.
- Chronic Villus Sampling (CVS): Typically done between 11 and 13 weeks of pregnancy, this procedure involves collecting a small piece of the placenta.
- Preimplantation Genetic Testing: Similar genetic testing can also be done before a couple gets pregnant if they choose to undergo in-vitro fertilization (IVF). This would involve combining eggs and sperm from a couple in a laboratory setting. The resulting embryos would then be tested to determine if they have a variant in the RS1 gene. Couples then chose the embryo that they would like to use to continue their pregnancy.
Emotional and Social Implications
A diagnosis with X-linked retinoschisis can have emotional and social implications on individuals and families. At the time of initial diagnosis, there may be feelings of shock and sadness for some parents[10]. Some mothers who unknowingly carried the affected RS1 gene may feel some guilt for passing it on to their children. It may also be difficult for some individuals to accept that they may not be able to drive, should not play contact sports and may become blind later in life. Conversely, families have also been known to have seen increased gratitude, empathy, and family cohesion after a diagnosis of XLRS[10]. It is important to note that every individual and family will live with and cope with XLRS differently. Seeking out a genetic counsellor may help individuals to cope with any emotions that they may be feeling that stem from their experience with XLRS.
Resources
- https://www.fightingblindness.org/diseases/x-linked-retinoschisis-xlrs
- https://www.cnib.ca/en?region=bc
- https://www.fightingblindness.org/newly-diagnosed
- https://www.fightingblindness.org/low-vision
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 Sieving, P. A., MacDonald, I. M., & Hoang, S. (2003 [Updated 2020 Nov 5].). X-Linked Congenital Retinoschisis. In M. P. Adam, H. H. Ardinger, R. A. Pagon, S. E. Wallace, L. J. H. Bean, K. W. Gripp, G. M. Mirzaa, & A. Amemiya (Eds.), GeneReviews(®). Seattle (WA): University of Washington, Seattle
- ↑ 2.0 2.1 Molday, L. L., Hicks, D., Sauer, C. G., Weber, B. H. F., & Molday, R. S. (2001). Expression of X-Linked Retinoschisis Protein RS1 in Photoreceptor and Bipolar Cells. Investigative Ophthalmology & Visual Science, 42(3), 816-825.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Sikkink, S. K., Biswas, S., Parry, N. R., Stanga, P. E., & Trump, D. (2007). X-linked retinoschisis: an update. J Med Genet, 44(4), 225-232. doi:10.1136/jmg.2006.047340
- ↑ 4.0 4.1 Retina. (2020). Retrieved from https://www.aao.org/eye-health/anatomy/retina-103
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 George, N. D., Yates, J. R., & Moore, A. T. (1996). Clinical features in affected males with X-linked retinoschisis. Arch Ophthalmol, 114(3), 274-280. doi:10.1001/archopht.1996.01100130270007
- ↑ 6.0 6.1 6.2 6.3 6.4 Lee, B. (2022). X-linked Retinoschisis. Retrieved from https://eyewiki.aao.org/X-linked_Retinoschisis#cite_note-9
- ↑ Apushkin, M. A., & Fishman, G. A. (2006). Use of dorzolamide for patients with X-linked retinoschisis. Retina, 26(7), 741-745. doi:10.1097/01.iae.0000237081.80600.51
- ↑ Zhang, L., Reyes, R., Lee, W., Chen, C. L., Chan, L., Sujirakul, T., Tsang, S. H. (2015). Rapid resolution of retinoschisis with acetazolamide. Doc Ophthalmol, 131(1), 63-70. doi:10.1007/s10633-015-9496-8
- ↑ Nussbaum, R. L., McInnes, R. R., Willard, H. F., & ebrary, I. (2016). Thompson & Thompson genetics in medicine (Eighth ed.). Philadelphia: Elsevier.
- ↑ 10.0 10.1 Turriff, A., Nolen, R., D'Amanda, C., Biesecker, B., Cukras, C., & Sieving, P. A. (2020). "There Are Hills and Valleys": Experiences of Parenting a Son With X-Linked Retinoschisis. Am J Ophthalmol, 212, 98-104. doi:10.1016/j.ajo.2019.11.023