Course:MEDG550/Student Activities/Huntington's Disease
Huntington's Disease (HD) is a genetic disease that affects a person's body, mind, and mood.[1][2] The disease causes breakdown of cells in the brain. Huntington's is a progressive disease, meaning symptoms get more severe over time. People with HD usually show their first symptoms between the ages of 35 and 44 years old. Symptoms continue to develop and progress, and most individuals survive 15-18 years after the initial diagnosis.
Symptoms
People with Huntington's Disease will show some or all of the following features:[1][2][3]
Physical Features:
- Involuntary movements
- Rigid muscles
- Unusual walking style or difficulties walking
- Difficulty speaking
- Difficulty swallowing
- Weight loss
Mental Features:
- Difficulties in organizing, planning, and adapting to changes
- Changes in personality
- Aggressive episodes
- Depression or suicidal thoughts
Often the first symptoms an individual with HD will show are small changes in movements like twitching or fidgeting, or subtle changes in mood and mind like irritability and forgetfulness. Over time, these symptoms will become more severe and new symptoms will develop.
Genetics
Inheritance

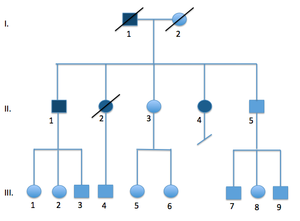
Each gene in the body is is present in two copies, one inherited from each parent.
HD is inherited in a pattern called autosomal dominant inheritance.[1] This means that a change in only one copy of a person's gene is enough to cause the disease.
If a person has Huntington Disease, they have a 50% chance of passing on a changed copy to each of their children. This means each of their children is at a 50% risk of Huntington's Disease. HD affects both men and women and can be inherited from either parent.
The HTT Gene
Huntington's disease is caused by extra letters in a gene called Huntingtin, or HTT for short [4]. The HTT gene was discovered in 1993 by the Huntington's Disease Collaborative Research Group[4]. Although many researchers have studied the HTT protein since then, its function is still unknown [3]. In HD, HTT accumulates in many brain structures, possibly explaining the wide range of symptoms that can occur.
HTT and Repeats
Genes are made up of strings of the letters A,C,G, and T, and use these letters as a code to make all the proteins needed for the body. The HTT gene has a region made up of many repeats of the letters "CAG" in a row. Most people have 26 or fewer CAGs in their HTT gene, while people with Huntington's have extra repeats.
Having extra CAG repeats in the gene changes the function of the protein made by the huntingtin gene, leading to symptoms of Huntington disease. The number of CAG repeats in the HTT gene determines whether a person has Huntington's Disease, and can also give hints about how early their symptoms will start to develop, and what the risk to their children is.
Sizes of Huntingtin Gene Repeats[2]:
| Name | Features | Number of repeats |
|---|---|---|
| Normal | Will NOT develop HD | <26 |
| Intermediate | Will NOT develop HD, but children are at risk | 27-35 |
| Reduced penetrance | May or may not develop HD, children are at risk | 36-39 |
| Full penetrance | Will develop HD, children are at risk | >40 |
| Juvenile onset | Will develop HD at a young age | >60 |

If a person has a "medium" amount of repeats (intermediate size), they may not develop the disease themselves, but their children are at a higher risk of HD[5]. This is because of a process called "anticipation."[3] Anticipation means that the disease starts earlier or is more severe as it is passed down over generations(e.g. a man may start showing symptoms at 55, while his grandson starts to show symptoms at 35). This is caused by increased number of CAG repeats from one generation to the next. Larger repeats are associated with younger age of onset and more severe disease.
Increase in the number of repeats usually occurs in men, but not in women. This means that a man with an intermediate sized repeat is more likely to have a child with Huntington disease than a woman with an intermediate sized repeat. Larger repeats are more unstable and have a higher chance of expanding in the next generation[6].
Adding more repeats to the HTT genes happens as a mistake. When our cells grow and divide, all of our genes are copied. Areas with repeats are more prone to mistakes than gene areas without repeats. Adding extra CAGs when copying the HTT gene can be thought of as similar to a child accidentally adding extra letter S's when copying out the word "Mississippi".
Prevalence and Population Frequency
Approximately 1 in 10,000 people are affected with Huntington's disease.[7]
Diagnosis
Many cases of HD are diagnosed when a person seeks medical help for difficulties at work or performing regular tasks[2]. To diagnose Huntington's disease, doctors will look for the following features:
- Progressive motor challenges, difficulty with voluntary movement
- Change in personality, depression, loss of mental abilities
- A family history of Huntington's disease
The diagnosis is then confirmed by testing the Huntington gene.
After the initial diagnosis, a person is followed by a team of specialists that assess disease symptoms and progression over time.
Targeted testing of the HTT gene can also be done to determine the number of repeats a person has. This can confirm a suspected or established diagnosis, or it can be done prior to the onset of any symptoms (“predictive testing”). Predictive testing is available to individuals with a family history of HD and who are at risk of developing HD themselves.
Management
Huntington's disease does not have a cure[1]. Medications can be used to treat certain symptoms of HD and help maintain quality of life.
Drugs can reduce motor symptoms like involuntary movements and rigidity, but they often have negative side effects (nausea, headaches) or can cause other types of motor problems. Particularly, drugs used to treat Parkinson's Disease (L-DOPA containing medications) should be avoided as they can increase involuntary movements in HD patients[2]. Smoking and alcohol consumption should also be avoided. Depression, aggression, and psychotic symptoms can be managed with psychotherapy and anti-depressive, anti-psychotic or mood-stabilizing medications. Participation in research or clinical trials for potential new treatments can also be an option.
Persons with HD need significant supportive care as they lose their ability to function independently[2]. Speech therapy, physical therapy, and occupational therapy can help manage and adapt to declining physical abilities. Emotional support and counselling can be beneficial to a person with HD as well as to their family or caregivers.
Genetic Counselling
Predictive Testing
People at risk for Huntington's disease can be seen in a medical genetics clinic for predictive testing. Predictive testing looks to see if a person will develop Huntington's before any symptoms appear. However, very few families at risk for Huntington's choose to have predictive testing [8].
Many factors contribute to the decision of whether or not to be tested, including (but not limited to):
- Living with uncertainty of not being tested
- Choosing whether or not to have children
- Planning for career, retirement, or care-taking
- Expectations and reactions of family members
- Fear of coping with a positive result
- Lack of preventative treatments
Learning that a person will or will not develop Huntington's disease in the future can both have significant impacts on the person and their family [8]. Reactions to testing can include depression, suicidal thoughts, regret over past decisions, loss of hope, freedom from uncertainty, relief or survivor’s guilt. They may also experience changes in their relationships or discrimination from other people.
Because individuals can react and cope in very different ways, the decision to test is a very personal one.
The genetic testing process involves three genetic counselling sessions to ensure the person is prepared for testing.[9] In the first appointment, the patient learns about the test and the condition, and is then given a minimum of one month to decide whether or not they want testing. At the second appointment, testing can be The test is done after the second session. Results are given at the final session, and the genetic counsellor can provide post-test counselling to arrange follow-up care and support.
Testing is only offered for adults over 18 years of age[9]. The American College of Medical Genetics does not recommend testing children for adult-onset conditions like HD[10]. Since there is no way to prevent or cure HD, there is no medical benefit to knowing whether a child will develop the disease later in life. Instead, testing should wait until the child is older so that he or she can make their own decision.
Reproductive Choices
Some families choose different reproductive options to avoid passing HD on to their children if they know that the disease runs in the family [9]. Once pregnant, the couple can test the fetus's HTT gene and may choose to terminate the pregnancy if the test shows the fetus would develop Huntington's in the future. Other couples use IVF (in vitro fertilization) to create a number of embryos and test each one for Huntington disease (called Preimplantation Genetic Diagnosis, or PGD). Only unaffected embryos are then used to get pregnant. Other options include the use of donor eggs or sperm, adopting a child from another family, or choosing not to have children.
Family Members
HD can also be very difficult on a person’s family, spouse, or caregiver, and a diagnosis can be devastating for those individuals as well as for the patient[2][8]. Family members find it hard to manage their loved one’s changing personality and increasing dependence. Eventually, the affected person becomes totally reliant on their caregivers. It is therefore important to connect families with sources for practical and emotional support.
Distress for family members can be complicated by the knowledge that they also may be at risk to have inherited a genetic change that will lead to development of Huntington's disease. This risk may be too stressful for some families, leading people to deny the existence of Huntington's disease in their family and avoid treatment or testing.[11] Genetic counselling for the entire family can clarify risks and help family members to make their own decisions about predictive testing.
Insurance and Discrimination
In Canada, the Genetic Non-Discrimination Act makes it illegal for companies to request or require the results of genetic testing.[12] The goal of the law is to allow individuals to choose whether or not to get genetic testing based on their own priorities and values, rather than avoiding testing out of fear of discrimination from insurance or employment.
Resources
Huntington Society of Canada: http://www.huntingtonsociety.ca
International Huntington Association: http://www.huntington-assoc.com
HDBuzz: http://en.hdbuzz.net
Enroll-HD (a worldwide observational study of Huntington disease families): https://www.enroll-hd.org/
To locate a genetics clinic near you, speak to your primary health care provider or visit www.cagc-accg.ca (Canada) or www.nsgc.org (United States).
References
- ↑ 1.0 1.1 1.2 1.3 Walker, F.O. (2007). Huntington's Disease. Lancet 369:218-28.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Warby SC, Graham RK, Hayden MR. Huntington Disease. (1998 [Updated 2014 Dec 11]). In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2015. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1305/
- ↑ 3.0 3.1 3.2 Zheng, Z. & Diamond, M.I. (2012). Huntington Disease and the Huntingtin Protein. Progress in Molecular Biology and Translational Science. 107:189.
- ↑ 4.0 4.1 The Huntington's Disease Collaborative Research Group. (1993). Cell. 72:971-983.
- ↑ Semaka, A., Kay, C., Doty, C., Collins, J.A., Bijlsma, E.K., Richards, F., Goldberg, Y.P. & Hayden, M.R. (2013). CAG size-specific risk estimates for intermediate allele repeat instability in Huntington disease. J Med Genet. 50:696-703.
- ↑ Wheeler, V.C., Persichetti, F., McNeil, S.M., Mysore, J.S., Mysore, S.S., MacDonald, M.E., Myers, R.H., Gusella, J.F., Wexler, N.S., The US-Venezuela Collaborative Research Group. (2007). J Med Genet. 44:695-701.
- ↑ Baine, F.K.; Krause, A.; Greenberg, L.J. (2016). "The frequency of Huntington disease and Huntington disease-like 2 in the South African population". Neuroepidemiology. 46 (3): 198–202.
- ↑ 8.0 8.1 8.2 Crozier, S., Robertson, N. & Dale, M. (2015). The psychological impact of predictive genetic testing for Huntington's Disease: a systematic review of the literature. J Genet Counsel. 24:29-39.
- ↑ 9.0 9.1 9.2 MacLeod, R., Tibben, A., Frontali, M., Evers-Kiebooms, G., Jones, A., Martinez-Descales, A., Roos, R.A., & Editorial Committee and Working Group 'Genetic Testing Counselling' of the European Huntington Disease Network. (2013). Clin Genet. 83:221-231.
- ↑ Committee of Bioethics, Committee on Genetics, The American College of Medical Genetics & Genomics Social, Ethical and Legal Issues Committee. (2013). Ethical and policy issues in genetic testing and screening of children. Pediatrics. 131:620.
- ↑ Migliore, S.; Jankovic, J.; Squiteri, F. (2019). "Genetic counseling in Huntington's disease: potential new challenges on horizon?". Frontiers in Neurology. 10 (453).
- ↑ "Genetic Non-Discrimination Act (S.C. 2017, c.3)". Justice Laws Website, Government of Canada. 2017.