Course:MEDG550/Student Activities/Glucose 6-Phosphate Dehydrogenase Deficiency
Glucose 6-Phosphate Dehydrogenase (G6PD) is an enzyme found in red blood cells, which carry oxygen from the lungs to all the cells of the body. G6PD deficiency is a common genetic condition where red blood cells do not have enough of the G6PD enzyme, which can lead to certain medical issues. G6PD deficiency affects males more frequently than females. However, many people with the deficiency do not show symptoms of the disorder.
Clinical Features
Hemolytic Anemia
Most people with G6PD deficiency are asymptomatic, meaning they do not show signs of the disease and usually do not have any medical issues. However, they do have a lower level of G6PD enzyme, so they are susceptible to episodes of “hemolytic anemia”. That means that the body doesn’t have enough red blood cells (anemia) because the cells are breaking down (hemolysis) faster than the body can make more.[1]
The reason that the red blood cells die more quickly than they should is because the G6PD enzyme is part of a pathway that produces molecules to protect the cell against oxidative damage[2]. When a person with G6PD deficiency is exposed to a substance that causes oxidative stress, their red blood cells are not able to defend against that stress and the cells become damaged. Most cells have a number of pathways that can produce these protective molecules, but red blood cells only have the G6PD pathway for this task[1], which is why only red blood cells are affected by this condition. Substances that can cause this oxidative stress include some medications (including anti-malaria drugs, some chemotherapeutics, and more), acute infections (fever), or even certain foods such as fava beans.
Symptoms of an acute episode of hemolytic anemia include:
- Fatigue
- Pale skin
- Rapid breathing or shortness of breath
- Back and/or abdominal pain
- "Hemoglobinuria" (dark yellow/orange or red urine due to passing the hemoglobin from the dead red blood cells)
- Mild jaundice (yellowing of the skin or whites of the eyes)
Neonatal Jaundice
Although the reason is not known, newborn babies with G6PD deficiency have a greater chance of experiencing neonatal jaundice[1]. This is caused by too much bilirubin in the body, which is a molecule that is normally found and is usually cleared by the liver. It is normal for newborns to have higher levels of this molecule and it can cause their skin to look yellow. However, in some babies, the bilirubin levels are too high and need to be treated. If left untreated for too long, high bilirubin levels can cause brain damage ("encephalopathy") and lead to intellectual disability[1].
Prevalence
An estimated 4.9% of people worldwide have G6PD deficiency, roughly 400 million people.[3] It is the most common enzyme deficiency. G6PD deficiency occurs much more frequently in individuals of certain backgrounds. It is seen most frequently in individuals from certain parts of Africa, Asia, the Mediterranean, and the Middle East. G6PD deficiency is thought to occur more often in these areas because it confers some protection against malaria.[3] G6PD deficiency occurs more frequently in males than females.[1]
Diagnosis
Testing for G6PD deficiency should be considered in individuals of African, Middle Eastern, or Asian descent with signs of hemolytic anemia, males with a family history of jaundice, and newborns who have severe jaundice.[4]
G6PD deficiency can be diagnosed in a few different ways. Most often it is diagnosed by a blood test which then looks at the activity of the G6PD enzyme.[5] If the enzyme levels are found to be below a certain threshold a diagnosis will be made. Genetic testing is not routinely used in diagnosing G6PD deficiency initially in an individual with symptoms but can be used to confirm a diagnosis or offer testing to family members who are asymptomatic but may have a chance of having G6PD deficiency.[5]
Management
The best way to manage G6PD deficiency is by avoiding certain medications and foods to prevent the onset of a hemolytic episode[1]. For a complete and updated list of substances to avoid, see this table that is managed by the G6PD Deficiency Association. Acetaminophen (Tylenol), and diphenyldramine (Benadryl) can likely be taken at low doses with careful monitoring for individuals who do not have severe forms of G6PD deficiency.[5] It is important to consult with your doctor and pharmacist before taking new medication.
In the event of a hemolytic anemia episode removal and avoidance of further triggers, and supportive care is the typical treatment course.[5] Once the trigger is removed symptoms typically resolve within a few weeks.
However, if a severe episode of anemia occurs, it can be treated by:
- Surveillance by a doctor
- Folic acid and iron supplements to help restore hemoglobin levels
- Blood transfusion, if necessary
Neonatal jaundice caused by G6PD deficiency is treated like any other form of jaundice. Phototherapy (exposure to light) is effective in most cases; in extreme cases, the baby may require a blood transfusion[2].
Genetics & Inheritance
G6PD deficiency is caused by a change in the G6PD gene that causes the gene not to work properly. This means that the body's cells cannot produce enough G6PD enzyme.
Inheritance
Humans have 46 chromosomes in each of their cells: 22 pairs of regular chromosomes and 1 pair of sex chromosomes. Females typically have 2 Xs for their sex chromosomes and males typically have 1 X and 1 Y. You inherit 1 copy of each chromosome pair from each of your parents.
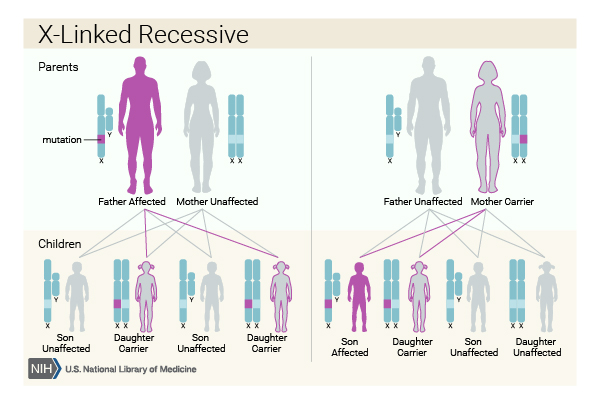
The genetic change or "mutation" that causes G6PD deficiency is passed down through an inheritance pattern called "X-linked recessive"[2]. This means that G6PD is found on the X chromosome, and the genetic change needs to be found on all X chromosomes in your cells to cause the disorder. Because males only have 1 X chromosome, they only have 1 copy of the G6PD gene. If that copy has a change in it, they will have G6PD deficiency.
Females, on the other hand, have 2 X chromosomes. A working copy of the gene on 1 X chromosome can compensate for a copy with a change in it on the other X chromosome. This would make someone a "carrier" for G6PD deficiency, but will not cause her to have the disease. However, a female can get G6PD deficiency if both of her parents pass on an X chromosome with a genetic change in that gene. This means that females get G6PD deficiency much less frequently than males.
Males with G6PD deficiency have a chance of passing on their non working copy of the G6PD gene. Because males pass on their Y chromosome and not their X chromosome to their sons, all of their sons will not inherit the change and will not have G6PD deficiency. Males pass on their X chromosome to their daughters. All daughters of men with G6PD deficiency will be carriers. Carriers are unlikely to show symptoms of G6PD deficiency because they still have one working copy of the gene but they would be able to pass on the non working copy to their own children.
Females who are carriers have on working copy and one working copy of the G6PD gene. Women will pass on one of their two X chromosomes to their children. Which X chromosome is passed on is random. If a female carrier has a child with an unaffected male their is a 25% chance that he would pass on his Y chromosome and she would pass on her X chromosome with the non working copy of the G6PD gene. This means she has a 1/4 or 25% chance of having a son with G6PD. There is also a 25% that the father would pass on his Y chromosome and she would pass on her X chromosome with a working copy of the G6PD gene. This means there is a 25% chance of having a son who does not have G6PD deficiency. There is a 25% chance the father will pass on his X chromosome with a working copy of the G6PD gene and she will pass on her X chromosome with the working copy. This is a 1/4 or 25% chance of having an unaffected daughter. There is also a 25% chance she would pass on her X chromosome with the non working copy of the G6PD gene and her partner passes on his X chromosome in which case the daughter would be a carrier. Just like her carrier mother, she would like not show symptoms of G6PD but would be able to pass on the non working copy of the gene to her own children.
Here is a diagram to help explain how it works:
Genetic Counselling
There are many different mutations in the G6PD gene that cause all G6PD deficiency. Some are relatively common in certain geographical regions. For example, the "Mediterranean" mutation is more common in Italy, Spain, Greece, the Middle East and India[2]; the "A-" mutation is more common in southern Europe and Africa[2]; and the "Canton" mutation is more common in China[2]. These mutations are often inherited and can cause asymptomatic G6PD deficiency or may lead to episodes of acute hemolytic anemia.
However, mutations can also happen randomly in someone instead of being passed down from that person's parents, which are called "de novo" ("new") mutations. New mutations usually cause a more severe form of G6PD deficiency where the person experiences chronic hemolytic anemia (rather than acute episodes) and may be dependent on blood transfusions throughout their life[1]. People with severe, chronic forms of G6PD deficiency may consider prenatal diagnosis when they are having children.
Genetic counselling may be a good option for people with a family history of G6PD deficiency. A genetic counsellor can review your family history, explain your chances of being having G6PD deficiency or having a child with G6PD deficiency, and discuss options including genetic testing. For more information on genetic counselling services near you, visit the Canadian Association of Genetic Counsellors (Canada) or the National Society of Genetic Counselors (USA).
Patient Resources
Here are some websites with more information on G6PD Deficiency. These are not intended to be used as medical advice. If you are worried or have questions about G6PD, talk to your doctor.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Mason PJ, Bautista JM, Gilsanz F. (2007). G6PD deficiency: the genotype-phenotype association. Blood Reviews. 21: 267-283.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Luzzatto L. (2006). Glucose 6-phosphate dehydrogenase deficiency: from genotype to phenotype. Haematologica. 91: 1303-1306.
- ↑ 3.0 3.1 Nkhoma, E.T.; Poole, C; Vannappagari, V; Hall, S.A.; Beutler, E. (2009). "The global prevalence of glucose-6-phosphate dehydrogenase deficiency: A systematic review and meta-analysis". Blood Cells, Molecules, and Diseases. 42 (3): 267–278.
- ↑ Frank, J.E. (2005). "Diagnosis and management of G6PD deficiency". Am Fam Physician. 72 (7): 1277–1282.
- ↑ 5.0 5.1 5.2 5.3 Bubp, J; Jen, M; Matuszewski, K (2015). "Caring for Glucose-6-Phosphate Dehydrogenase (G6PD)–Deficient Patients: Implications for Pharmacy". P T. 40 (9): 572–574.
- ↑ "What are the different ways in which a genetic condition can be inherited?" Genetics Home Reference. NIH U.S. National Library of Medicine, January 2017. 12 Jan 2017.