Course:MEDG550/Student Activities/Carnitine Uptake Deficiency
What is Carnitine Uptake Deficiency?
Carnitine (kahr-ni-teen) Uptake Deficiency (CUD) is when you have trouble making energy from fats (fatty acids) in your body. [1][2][3]
Carnitine is a substance that you need to help turn fats in to energy. Carnitine is mainly found in the food you eat.[4]
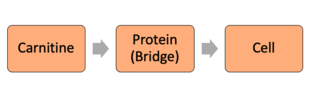
It is important for carnitine to enter your body's cells so that it can do its job in helping make energy for organs like your heart, muscles, and kidneys.[1] Normally, carnitine enters your body's cells through a protein that acts like a bridge. In CUD, not enough carnitine is able to enter your body's cells because the protein (bridge) is missing. With no bridge for carnitine to cross, there's less carnitine in cells and less fatty acids being turned in to energy.[1][2]
With CUD, it is only your ability to make energy from fats that is different from other people. You can still use sugars from food as an energy source for your body. This causes problems because your body needs to use fats for energy when it runs out of sugars (like when you have not eaten in a long time).[1]
Other names for Carnitine Uptake Deficiency
- Carnitine Uptake Defect
- (Systemic) Primary Carnitine Deficiency
- Carnitine Transporter Deficiency
What are the signs and symptoms of Carnitine Uptake Deficiency?[1][2][3]
The signs and symptoms for CUD can look different in every person. Some people show symptoms when they are born and some people can live their whole lives with no symptoms.
If you have symptoms, they can be mild or more serious. You may notice these symptoms during times when you need more energy like when you haven't eaten in a long time or you're feeling sick. If you're pregnant, you may begin to notice symptoms as your body needs more energy to support your pregnancy.
For children, signs and symptoms can include:
- Poor feeding
- Irritability/Confusion/Vomiting
- Feeling tired (fatigue)
- Low blood sugar
- Heart problems (weak heart)
- Muscle problems:
- Muscle weakness
- Low muscle tone (floppy muscle)
- Increased size of liver (hepatomegaly) and/or liver problems

For adults, signs and symptoms can include:
- Feeling tired (fatigue)
- Low blood sugar
- Heart problems
- Liver problems
- No symptoms
Both children and adults with CUD are at risk of coma or sudden death if left untreated.

How do you get Carnitine Uptake Deficiency?[2][5]
CUD is a genetic condition where the gene named SLC22A5 is not working. Every person has 2 copies of the SLC22A5 gene.
You get one copy of the gene from your mother and the other copy of the gene from your father. For you to get CUD, each of your parents has to give you a copy of the SLC22A5 gene that is not working.
Having at least 1 copy of the SLC22A5 gene that works from either your mother or father is all you need to not be affected by CUD.
If you have only have 1 working copy of the SLC22A5 gene, you are called a 'carrier' because you still carry 1 copy of the gene that does not work. Importantly, carriers don't show any symptoms of CUD.
How are you diagnosed with Carnitine Uptake Deficiency?[1][6]
CUD can be diagnosed through newborn screening, through looking at your skin cells, and through genetic testing. Men and women of all ethnic backgrounds can be diagnosed with CUD.
Newborn Screening[7]
In some parts of the world, CUD is included in newborn screening programs. Newborn screening is a blood test that can be done on newborn babies to test for conditions like CUD. To see if the baby has CUD, the test looks at carnitine levels in the blood.
If there are low levels of carnitine seen in the blood, it could mean one of the following:
- The baby has CUD
- The baby's mother has CUD (because during pregnancy mom is sharing her carnitine with baby)
- Both the baby and the mother has CUD
Following newborn screening, further tests are needed to confirm the blood test results and to see whether the baby and/or the mother have CUD.
Skin Cell Studies
The cells in your body tissue can be tested to see how much carnitine is able to enter your cells.[4] If there is a less than normal amount of carnitine entering cells, then that could be used to diagnose you with CUD.
Genetic Testing
A blood or saliva sample can be collected and tested to see if your SLC22A5 genes, the genes involved in CUD, are working or not. Genetic testing is usually done to confirm a suspected diagnosis of CUD.
How are you treated for Carnitine Uptake Deficiency?[1][2][3][4]
CUD is mainly treated by taking carnitine supplements every day.[1] Taking the carnitine supplements helps to prevent the signs and symptoms of CUD from happening. Sometimes people can have minor side effects with taking the supplements such as diarrhea and stomach pain. Your doctor can lower the dose you take if you experience side effects.[2]
Also, your doctor will arrange for you to see a dietician who will help you with what your diet should look like.[3] Managing your food intake is important to avoid experiencing symptoms. For example, you should avoid going long periods of time without food so you don't get low blood sugar.
Genetic Counselling for Carnitine Uptake Deficiency[4]
If you or a family member have been diagnosed with CUD, then you may want to be seen by a genetic counsellor. A genetic counsellor is a health professional that will help you understand and adapt to your or your family member's diagnosis of CUD.
Your genetic counselling appointment can include:
- A detailed medical and family history
- Helping you understand how CUD is a genetic condition
- Describing if and how CUD impacts your family
- The option of genetic testing
- Addressing concerns and providing support
- Family planning if you are thinking of having children
Genetic Counselling Issues: Prenatal Testing[4][8]
Prenatal testing is available as an option for you during your pregnancy if you or someone in your family has been diagnosed with CUD through genetic testing.[8] Prenatal testing would let you know if your baby is has CUD while you are pregnant. Knowing that your baby has CUD could help with preparing to take care of them. Prenatal testing does include some risks like miscarriage.
If you are worried about the risks that come with prenatal testing but would still like your baby tested for CUD, there is the option of newborn screening. It is important to remember that newborn screening is completed after your baby is born while prenatal testing happens when you are pregnant.
There is no right or wrong choice when deciding if you want your baby tested for CUD or not. Meeting with a genetic counsellor to discuss your options during pregnancy can help figure out what works best for you.
Patient Resources
Fatty Acid Oxidation Support Group
Adult Metabolic Diseases Clinic (Vancouver, B.C.)
Canadian Association of Genetic Counsellors: Find a Clinic Near You
National Society of Genetic Counsellors: Find a Genetic Counsellor Near You (Canada & USA)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Almannai, M., Alfadhel, M., & El-Hattab, A. W. (2019). Carnitine inborn errors of metabolism. Molecules (Basel, Switzerland), 24(18), 3251. doi:10.3390/molecules24183251.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Longo, N., Frigeni, M., & Pasquali, M. (2016). Carnitine transport and fatty acid oxidation. Biochimica Et Biophysica Acta. Molecular Cell Research, 1863(10), 2422-2435. doi:10.1016/j.bbamcr.2016.01.023
- ↑ 3.0 3.1 3.2 3.3 Merritt, 2., J Lawrence, Norris, M., & Kanungo, S. (2018). Fatty acid oxidation disorders. Annals of Translational Medicine, 6(24), 473-473. doi:10.21037/atm.2018.10.57
- ↑ 4.0 4.1 4.2 4.3 4.4 Magoulas, P. L., & El-Hattab, A. W. (2012). Systemic primary carnitine deficiency: An overview of clinical manifestations, diagnosis, and management. Orphanet Journal of Rare Diseases, 7(1), 68-68. doi:10.1186/1750-1172-7-68
- ↑ Urban, T. J., Gallagher, R. C., Brown, C., Castro, R. A., Lagpacan, L. L., Brett, C. M., et al. (2006). Functional genetic diversity in the high-affinity carnitine transporter OCTN2 (SLC22A5). Molecular Pharmacology, 70(5), 1602-1611. doi:10.1124/mol.106.028126
- ↑ Frigeni, M., Balakrishnan, B., Yin, X., Calderon, F. R. O., Mao, R., Pasquali, M., & Longo, N. (2017). Functional and molecular studies in primary carnitine deficiency. Human Mutation, 38(12), 1684-1699. doi:10.1002/humu.23315
- ↑ El-Hattab, A. W., Li, F., Shen, J., Powell, B. R., Bawle, E. V., Adams, D. J., et al. (2010). Maternal systemic primary carnitine deficiency uncovered by newborn screening: Clinical, biochemical, and molecular aspects. Genetics in Medicine, 12(1), 19-24. doi:10.1097/GIM.0b013e3181c5e6f7
- ↑ 8.0 8.1 Tan, J., Chen, D., Li, Z., Yuan, D., Liu, B., Yan, T., et al. (2019). SLC22A5 gene mutation analysis and prenatal diagnosis for a family with primary carnitine deficiency. Zhonghua Yi Xue Yi Chuan Xue Za Zhi, 36(7), 690.