Course:GEOG352/Dushanbe: public health
The breakup of the Soviet Union in 1991 brought about a series of economic and social changes in the peripheral countries that once composed it. Tajikistan, a small country of 9 million is one of the most striking examples, located in the southernmost extremity of the former block. Today, more than half of its GDP consists of remittances sent home from migrants working primarily in Russia[1]. This has precipitated innumerable changes not only in the structure of institutions and the economy of the country, but also in the social relations and hierarchical dimensions of Tajik society.
Chief among these transformations is the healthcare system in Dushanbe, whose urban expansion has exacerbated the issues posed by outdated infrastructure, as problems relating to sanitation, waterways, and the provision of medical services are perpetually compounded by the growing population density as well as the poor allocation of resources to the public service sector. Citizens seeking healthcare have faced many difficulties as a result of the decentralization away from the Soviet regime, and the transition to a system of governance prioritizing commerce economy over the service sector. Although Tajikistan's urban population is little over 25%[2], urban population density resulted in disease epidemics at the beginning of the century, and Dushanbe's highly centralized and faltering healthcare system is unable to cope with the problems that have arisen from the strain that significant population growth has placed on weakened systems of public infrastructure. This, coupled with the exodus of healthcare providers and influx of migrants has proven to be a major public health challenge in the Tajik capital. Rethinking the economic structure and allocation of resources is necessary to independently and durably remedy the problems.
Overview
Healthcare infrastructure in Dushanbe is an issue which straddles multiple scales. As a country, Tajikistan has suffered greatly from its post-Soviet decentralization and rapid privatization, and a following 5-year long civil war. Even now, much of the population struggles to maintain above-subsidy level incomes and cannot afford increasingly privatized healthcare provision. The constitution was amended in 2003 to remove the guarantee of free healthcare, further dividing the access gap. (European Observatory on Health Systems and Policies 2016)[3] Although recent efforts towards financial protection have been made, financial barriers remain one of the chief concerns for Tajiks in need.
It is in the urban scale of Dushanbe that this problem of accessibility manifests itself most vividly. People seeking medical aid from rural areas try to overcome the physical barrier by migrating to Dushanbe, and those of Dushanbe attempt to circumvent the financial barriers by migrating outwards from Tajikistan. This has tangible effects on the city’s demographic structure, especially when coupled with the spike of epidemics in Dushanbe, caused by poor water filtration, changing lifestyles, and transient populations.
The issues faced by Dushanbe and Tajikistan after the dissolution of the Soviet Union, namely difficulties surrounding adjustment to decentralization and privatization, are representative of similar issues faced by other Transition States. Many Central Asian states struggle to adequately operate water treatment plants when both consumer tariffs and central government subsidies are insufficient. The resulting deterioration in distribution networks and unreliable service provision are among the prominent causes of waterborne epidemics like Typhoid. (Tannerfeldt and Ljung 2006)[4]
Transition states are not “developing” in the same way as other states of the global South—most of them are not even part of the geographical global south, and rarely harbor the same kind of rapid urbanization. Nonetheless, their interest in attracting global capital for investment-driven development is similar, but for them it is accompanied by an alternate baggage that is their Soviet past. Dushanbe is among these municipalities and states that must simultaneously adapt its economy and healthcare system to increasingly liberal global economies, in order to facilitate the inevitable diversity and magnitude that accompanies a growing urban population.
Case Study
Public Health Infrastructure
While most of Tajikistan’s health workers are stationed in Dushanbe, the country as a whole only has 170 physicians per 100,000 residents compared to the European Union average of 347. Furthermore, there are only 444 nurses per 100,000 people in the country with the E.U having nearly double that (Khodjamurodov et al., 2016.). In terms of reforms in the context of human resources, emphasis has been placed on standardizing health education in order to make sure that it meets international standards. This issue can be seen as specific to Dushanbe, as it is home to Tajikistan’s largest medical school, The Abu Ali ibn Sino Institute of Medicine. This school was seen as having particularly lax admission standards which has arguably been a direct hindrance towards improving healthcare standards. Further compounding this issue, conflict that occurred in Dushanbe led to the emigration of approximately 1300 physicians (Coutsoukis, 2004[5])
In terms of tangible infrastructure in Dushanbe, the construction of new facilities in the mid 1990s was seriously backlogged, leading to many of them being considered substandard (Coutsoukis, 2004). only one drug treatment center with one hundred beds exists. The impact this has had on public health in the city is evidenced through the fact that it has the highest prevalence of the hepatitis C virus among intravenous drug users in Tajik cities. For emergency care, 43 ambulances have recently been purchased for use in Dushanbe. However, according to interviews with healthcare providers, transport by private vehicle is still more prevalent even in the case of symptoms such as chest pain and stroke (Khodjamurodov et al., 2016.). This suggests that there is a lack of public trust in the level of healthcare that the government can provide, even where it is most concentrated in Dushanbe.
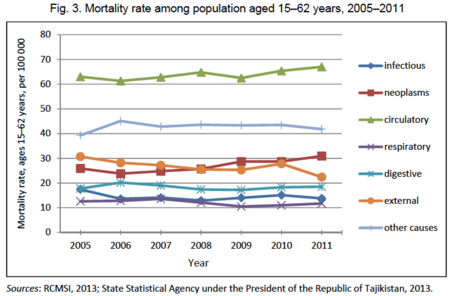
Diseases of Affluence
A foreigner to Tajikistan could hypothesize that as a developing country, the type of disease prevalent there would be those of so-called 'diseases of poverty', in other words communicable diseases associated with poor sanitation and the proliferation of bacteria and viruses. However, the transformation of livelihoods precipitated by the onset of Western lifestyle habits and diet makes the opposite true for Tajikistan, and particularly in Dushanbe. Indeed, the number one cause of premature death at 37% is cardiovascular (CVD) and particularly ishemic heart disease[6]. Nearly 60% of diseases are 'diseases of affluence', or Western diseases, including CVD, cancer, respiratory disease, and diabetes[7]. An interesting phenomenon is that most of these diseases are concentrated within the biggest cities of Tajikistan, notably Dushanbe[8]. This is understandable as the urban centers are the first point of arrival and convergence between various external cultures and novelties. At the time, the Soviet public health infrastructure was equipped mainly to address communicable diseases mostly present in rural areas as water sanitation and hygiene was not a problem in urban centers. However, given the deterioration of these infrastructures coupled with the lack of research or physicians able to competently handle these new diseases, people in urban centers with these new afflictions find other strategies to seek medical attention for their ailments[9], one of which will be discussed further down.
Communicable Diseases
Typhoid fever is a good example of a communicable disease which was an issue for the city of Dushanbe, Tajikistan[11]. The ailment mostly consists of fever and other adverse physical effects such as stomach pain and muscle aches. The 1997 Dushanbe population of 600,000 people was effected by the spreading of typhoid due to a failure in the public water sanitation system. Diagnosis of typhoid fever is defined as presence of S. Typhi in urine, blood or stool samples and in 1997 was recorded to be 10,776 cases during the period of January 1996 – July 1997 [12]. It was concluded via patient questionnaire that the cases were linked to the consumption of un-boiled water in 30 days prior to being diagnosed. The groups evaluation of the water supply, sourced from the Varzob River was found to contain silts and fecal material and that level increased when examining the taps of a collection of households, which suggests an issue with the water piping and filtration systems. Further commentary on the Typhi outbreak of 1997 states that one strain of the illness, phage type UVS was resistant to ciprofloxacin, ampicillin, chloramphenicol, and trimethoprim[13]. This resistant strain of Typhi that is perpetuated by an insufficient water system in Dushanbe has caused for recurrent outbreaks of the disease in the city and can be considered a truly epidemic disease. The parasite Plasmodium Falciparum is a malaria causing parasite that, due to the civil war in the country from 1992-1997 the ailing infrastructure in the area has been found to equal a malaria outbreak. This was reported to be likely due to limited access to laboratory services, which can be traced back to lack of supportive services after the disintegration of the Soviet Union. This was mostly due to the destruction of various infrastructures and facilities that provided the city of Dushanbe with preventative healthcare options for citizens, and therefore their absence allowed for the spreading and perpetuation of these disease outbreaks during the civil war period in Dushanbe and Tajikistan.
Medical Migration
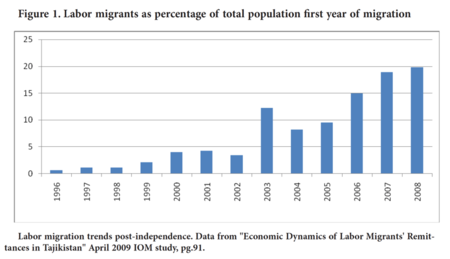
Since the end of the civil war, emigration from Tajikistan has gradually been growing. Most of the Tajik emigrants originate from rural areas, having previously been involved in agriculture, soviet industries, or livestock tending (IOM, 2009)[14]. This contrasts with people living in urban areas who tend to engage in bazar vending rather than resort to migration. The graph below illustrates the gradually increasing percentage of the population that has left the country for the first time in order to find work elsewhere since the end of the civil war until 2008.
Given Tajikistan's history within the former Soviet Union, Tajik labor migrants' well-established networks in Moscow, and the absence of a language barrier, it is unsurprising that one of the top destinations for Tajiks seeking medical care is Moscow. The gradual deterioration of the public health service has led to new strategies to receive medical care. As mentioned earlier, there is divergence in the type and occurrence of diseases in Tajikistan depending on the level of urbanization of the locality being studied. Migration of people seeking healthcare for certain medical conditions is strongly shaping the demographics of public health use in Tajikistan. In rural areas, people afflicted with communicable diseases migrate to Dushanbe to seek treatment such as vaccines, whereas those living in the capital leave the country (notably to Russia and India) to receive treatment for cancers and other such diseases, since the research and quality of infrastructures is underfunded and cannot respond adequately to these ‘new’ diseases related to rapidly changing lifestyle factors[16].
The Post-Soviet Reality
Tajikistan faces a challenging national public health situation in which its needs and its available resources seem almost impossible to reconcile. Existing health facilities are outdated and in need of maintenance, as they were constructed during the Soviet era, in which budgeting was more generous and 91% of Tajikistan’s GDP was received in the form of financial transfers from the Russian Central Bank[17]. In the new independent economic reality, Tajikistan’s per capita health spending has fallen to 47 USD, of which only a fraction is from the national government, placing it at the lowest in Central Asia and among the lowest in the world (Linn, J. 2005). In the absence of this funding, facilities have fallen into disrepair and have experienced reduced functionality as a result. Urban health facilities average 12 hours per day without heating in the winter and 5 hours per day without electricity[18]. Evidence of the public health consequences of Soviet absence can be seen in the current generation of children in Dushanbe, whose physical appearance shows them to be in worse health than their parents. Though the urban population suffers less than the rural, 30% of Dushanbe’s children appear to have moderately or severely stunted growth (Olcott, M. 2012). This is indicative of a problem that is both self-perpetuating and ingrained in Dushanbe’s urban social reality, as the coming generations face a greater degree of the same health issues as their forebears, with an increasingly inadequate system responsible for combatting said issues.
Lessons Learned
This case study of Dushanbe can be eye-opening when compared and contrasted with the expectations that we have grown through the course of the semester. The sanitation infrastructure in Dushanbe has deteriorated significantly since the end of the Soviet Union, and can be considered a catalyst in the degradation of preventative health care and medical support centres. Because of this, the city is susceptible to many types of disease outbreaks and lacks the proper services needed to quell the problem and treat the affected. On a larger scale we have found that Dushanbe is unique among many of the other major cities in the global south. It is geographically not situated in the global south, but in the north within what can be considered Eastern Europe and former Soviet Union territory. Its political and municipal instability, and historical baggage in the global liberal economy, can define Dushanbe as a type of developing city distinct from others in the geographic global south. The proliferation of western diseases is a testament to the possibility that Dushanbe had more stable state support and health infrastructure in its Soviet days, and the impossibility of a simple transition to a western-style free market. The Transition States will likely find a course of development unlike the Western powers or the Southern megacities, in a departure from ill-adapted shock treatment.
References
Reference List
- ↑ World Bank Group (2017). Tajikistan: Strong Growth with a Challenging Outlook. Country Economic Update. World Bank Group Macroeconomics & Fiscal Management.
- ↑ Tajikistan - Urban population (% of total). (n.d.). Retrieved April 07, 2018, from https://tradingeconomics.com/tajikistan/urban-population-percent-of-total-wb-data.html
- ↑ Khodjamurodov G, Sodiqova D, Akkazieva B, and Rechel B. (2016) Tajikistan: health system review. Health Systems in Transition, vol.18(1), pg. 91.
- ↑ Tannerfeldt, G. (2006) “More urban, less poor: an introduction to urban development and management.” London: Sterling, VA: Earthscan.
- ↑ Coutsoukis, Photius. (2004). Tajikistan Health Care system. [online] Photius.org. Available at: https://photius.com/countries/tajikistan/society/tajikistan_society_health_care_system.html
- ↑ Akkazieva, B., Tello, J., Smith, B., Jakab, M., Krasovsky, K., Sautenkova, N., Yuldasheva, L., Shoismatuloeva, M. (2014). Better noncommunicable disease outcomes: Challenges and opportunities for health systems. WHO Regional Office for Europe.
- ↑ Smith O, Nguyen SN (2013). Getting Better: Improving Health System Outcomes in Europe and Central Asia. Washington, DC: World Bank
- ↑ Akkazieva, B., Tello, J., Smith, B., Jakab, M., Krasovsky, K., Sautenkova, N., Yuldasheva, L., Shoismatuloeva, M. (2014). Better noncommunicable disease outcomes: Challenges and opportunities for health systems. WHO Regional Office for Europe
- ↑ Smith O, Nguyen SN (2013). Getting Better: Improving Health System Outcomes in Europe and Central Asia. Washington, DC: World Bank
- ↑ Akkazieva, B., Tello, J., Smith, B., Jakab, M., Krasovsky, K., Sautenkova, N., Yuldasheva, L., Shoismatuloeva, M. (2014). Better noncommunicable disease outcomes: Challenges and opportunities for health systems. WHO Regional Office for Europe
- ↑ Epidemic Typhoid Fever - Dushanbe, Tajikistan, 1997. (1998, September 18). Morbidity and Mortality Weekly Report, 47(36), 752. Retrieved from http://link.galegroup.com/apps/doc/A21162140/HRCA?u=ubcolumbia&sid=HRCA&xid=81d03bdd
- ↑ Threlfall, E., Murdoch, D., Banatvala, N., Bone, A., Shoismatulloev, B., & Ward, L. (1998). Epidemic ciprofloxacin-resistant salmonella typhi in tajikistan. The Lancet, 351(9099), 339-339. 10.1016/S0140-6736(05)78338-0
- ↑ Pitt, S., Pearcy, B., Stevens, R., Sharipov, A., Satarov, K., & Banatvala, N. (1998). War in tajikistan and re-emergence of plasmodium falciparum. The Lancet, 352(9136), 1279-1279. 10.1016/S0140-6736(98)00040-3
- ↑ IOM (2009). Abandoned wives of Tajik Labor Migrants. IOM Study on the socio-economic characteristics of abandoned wives of Tajik labor migrants and their survival capabilities. Dushanbe: IOM.
- ↑ IOM (2009). ECONOMIC DYNAMICS OF LABOUR MIGRANTS’ REMITTANCES IN TAJIKISTAN. International Organization for Migration.
- ↑ Akkazieva, B., Tello, J., Smith, B., Jakab, M., Krasovsky, K., Sautenkova, N., Yuldasheva, L., Shoismatuloeva, M. (2014). Better noncommunicable disease outcomes: Challenges and opportunities for health systems. WHO Regional Office for Europe.
- ↑ Linn, J. (2005). Central Asia Human Development Report. Bringing down barriers: Regional cooperation for human development and human security. UNDP.
- ↑ Olcott, M. (2012) Tajikistan's Difficult Development Path. Carnegie Endowment for International Peace.
| This urbanization resource was created by Course:GEOG352. |