Documentation:FIB book/Ulnar Collateral Ligament (UCL) Injuries in Baseball
Abstract
Injury of the Ulnar Collateral Ligament (UCL) is extremely common in the sport of baseball despite it being rare in the general population. Almost a quarter of professional pitchers have had surgical UCL reconstruction, and injury prevalence is increasing dramatically among younger players. This review summarizes the biomechanical knowledge of the UCL injury. Human volunteer studies showed that the UCL contributed ~34.6 N-m of varus torque to resist valgus motion. From reviewing various cadaver studies, it was found that the injury threshold for UCL is significantly lower in cyclic loading than in ultimate testing. Additionally, cadaveric studies indicate that UCL damage is a major contributor to joint laxity and ulnar nerve strain. Major discrepancies were identified between injury tolerances from cadaveric studies and injury tolerances from human volunteer studies, which should be a priority for further studies. Lastly, we found a notable lack of research using computer simulation alone to study the UCL joint during throwing, which is an area for further study.
Introduction

Baseball is often referred to as ‘America’s national pastime’, and in recent years even young players have begun training year-round for the sport. Unfortunately, baseball players are a major at-risk population for Ulnar Collateral Ligament (UCL) injuries, alongside wrestlers, javelin throwers, tennis players, and football players[1]. The increase in year-round training (among other factors) has led to a twofold increase in the number of UCL reconstructions performed in professional athletes, 4 times as many in collegiate athletes, and 6 times as many in high school athletes. Generally, pitchers with UCL tears must undergo Tommy John surgery, which can require up to 2 years of recovery time.
The UCL joint is shown in Figure 1. The repetitive throwing motion required in baseball puts significant valgus stress on the elbow joint which can cause tearing both chronically and acutely.[2] The UCL injury from throwing is generally well-researched. This is because human volunteers are often available on university campuses, and the injury has an enormous impact on Major League Baseball. However, there are areas that require further research, such as modelling the elbow joint using computer simulation, and additional standardized cadaver testing. Therefore, this review aims to summarize the current body of research and prompt additional exploration of some key areas of study.
Basic Anatomy of the UCL Complex

The ulnar collateral ligament (UCL), also referred to as the medial ulnar collateral ligament (MUCL), is the anterior bundle of three ligaments that form the medial ulnar collateral ligament complex, along with the posterior bundle and the transverse ligament. The UCL is composed of two separate bands (anterior and posterior) that provide reciprocal function[2]. The anterior band of the anterior bundle is most taut during lesser degrees of flexion (30° to 90°), whereas the posterior band is most taut at higher degrees of flexion (60° to 120°)[1], as shown in Figure 2.
The UCL has been shown to be the primary stabilizer of the elbow in valgus stress, which occurs when the UCL experiences an oblique displacement away from the midline. The posterior bundle is a soft tissue stabilizer used greatest during flexion. While the transverse ligament was thought to contribute insignificantly to elbow stability, more recent literature has shown that the direct insertion of the transverse ligament onto the UCL could potentially play a role in elbow stability[2].
The origin of the UCL is posterior to the elbow’s axis of rotation, on the anterior, inferior, and lateral aspect of the medial epicondyle. The insertion of the UCL was generally believed to be solely onto the sublime tubercle, but recent studies have shown the UCL insertion to be a longer, distally tapered area that follows the ulnar ridge[2].
The UCL is the strongest of the elbow ligaments[2]. The valgus moment placed on the elbow during pitching is commonly the cause of UCL injury. The patient with a UCL injury will typically recall an acute “pop” felt or heard at the medial elbow during the overhand throw[1]. Valgus instability can cause pain, reduced accuracy, and decreased velocity[2].
The overhand throw as it relates to pitching can be divided into 4 stages: windup, cocking, acceleration, and follow-through[1], as shown in Figure 3. The UCL is commonly injured in overhead throwing athletes when the shoulder reaches a position of maximal external rotation during the transition of the cocking phase to the acceleration phase.
Epidemiology

This section will summarize the findings of epidemiological studies associated with UCL injuries in pitchers. These findings compare the increasing prevalence and severity of UCL injuries in overhand throwing and contact sports, and the relationship between MLB rules that exacerbate these injuries. Statistics are provided for reconstruction surgery to illustrate the consequences of UCL injuries in pitchers.
The prevalence of UCL injuries is thought to be low in the general population, only becoming a significant problem in overhand throwing and contact sports. This injury can be found in wrestlers, javelin throwers, tennis players, football players, and baseball players, with the highest incidence of UCL injuries occurring in professional pitchers[1]. Pitchers who are taller, heavier, have a greater workload, or are fatigued have a greater risk of UCL tears[3].
Research from 2 consecutive 5-year periods, 1995–1999 versus 2000–2004, identified a twofold increase in the number of UCL reconstructions performed in professional athletes, 4 times as many in collegiate athletes, and 6 times as many in high school athletes. A factor contributing to this relative epidemic of UCL injuries is the rise in unrelenting overuse due to institution of fall and winter seasons, indoor pitching camps, and participation with multiple teams[1]. The National Collegiate Athletic Association (NCAA) recorded 109 UCL injuries from 25 varsity sports between 2010 and 2014: Of these injuries, UCL injuries from throwing sports were more severe than from contact sports, leading to more rehabilitation time and reconstruction surgeries. As a result, throwing athletes demonstrated a significantly higher proportion of severe injuries than contact athletes[4], leading to the higher incidence of UCL injuries at professional sports levels.
A UCL tear is usually repaired with a surgical reconstruction procedure - the Tommy John surgery. Out of 78 pitchers who had UCL reconstruction between 1998 and 2003, 89% of these pitchers returned to play within 10–49 months of their injury. In terms of performance, pitcher earned run average returned to pre-injury levels within 2 years of return to play[3].
UCL injuries, particularly in baseball, have become increasingly common amongst athletes across a range of expertise levels due to changes in training seasons, rule changes, and reconstructive procedures. These injuries have especially affected professional pitchers’ loss of total play time and recovery process.
Study Methods and Key Findings
The mechanisms at which the UCL complex is loaded and ultimately injured can be studied using several methods. Firstly it is important to understand the biomechanics of a pitcher throwing a baseball and what kind of loads and strains are subjected to the elbow. This is best achieved through using human subject volunteers. Additionally, the failure mechanisms of the ligament should be assessed by use of cadaveric testing. Lastly, the use of computer simulations can help to understand the injury modes of the UCL in addition to determining critical loads.
Human Volunteer Experiments
Human volunteer testing is performed to understand the typical loads which a pitcher exerts on various points of the arm and shoulder. These studies typically recruit healthy athletes, usually in college, who are asked to throw a set of pitches which adheres to a testing protocol[5]. Selection criteria for a healthy pitcher usually include that they had not undergone surgery within the last 12 months, and that their pitch velocity measured to a certain threshold when thrown in the strike zone. This volunteer criteria ensured that high quality data was collected in terms of the pitcher’s ability to throw at a competitive level while maintaining a statistically significant number of subjects.
Volunteers are typically asked to follow their regular warm up routine and throw maximum effort pitches while filtering for anomaly pitches such as pitches out of the strike zone and low velocity pitches. Dynamic data may include: angular displacement, velocity, force and torque at the shoulder and elbow joints. As performed by Fleisig et Al., inverse dynamics calculations were used to solve for forces using measured kinematic data[5]. The elbow torque data can be broken up into a flexion-extension and varus-valgus components and the force data can be categorized as medial, anterior and compressive loads. Once the data is processed, the spatial coordinates which the maximum loads are experienced are found with margin between the subjects. These coordinates may include flexion, rotation, abducted and horizontal angles. In Fleisig’s study the maximum loads were experienced when the elbow was flexed 95° ± 10°, externally rotated 165° ± 11°, abducted 94° ± 21°, and horizontally adducted 11° ± 11°[5]. The following shows the maximum forces and torques produced at this instant.
| Parameter | Value |
|---|---|
| Varus Torque (Nm) | 64 +/- 12 |
| Flexion Torque (Nm) | 16 +/- 16 |
| Medial Force (N) | 300 +/- 60 |
| Anterior Force (N) | 160 +/- 80 |
| Compressive Force (N) | 270 +/- 120 |
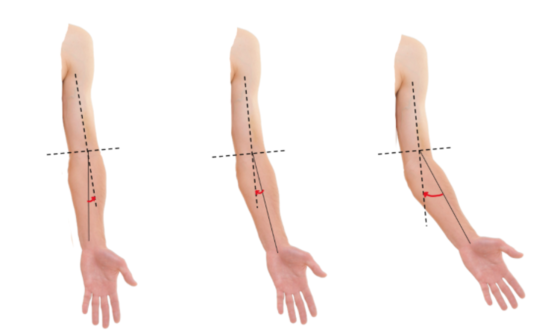
The implications of this data can be compared with other studies to understand the margins at which failure can occur. Since the UCL’s contribution to resist valgus motion could not be measured invasively from human volunteer subjects, cadaveric studies were referred to. For an example, this study compared results to the cadaveric study showing that “the ulnar collateral ligament (UCL) generated 54% of the varus torque needed to resist valgus motion” when the elbow was flexed 90 degrees[5]. Directions of varus and valgus motion are shown in Figure 4. Given a mean varus torque of 64 N-m, the UCL’s contribution can be scaled down to 34.6 N-m of varus torque to resist valgus motion. These values can be further compared to cadaveric testing to assess how close the maximum effort pitching data is from rupture or other failure modes of the ligament complex.
Cadaver Experiments
Cadaveric testing has been used to determine the maximum valgus torque on the UCL that causes both ultimate failure and cyclic failure, as well as to determine UCL contribution to joint laxity and ulnar nerve strain in the elbow. However, available literature regarding failure of the elbow is often contextualized by a comparison against performance of various UCL reconstruction methods. For the purposes of this literature review, only data pertaining to the native UCL will be considered.
One landmark study from Paletta et al constrained the elbow at 30˚ flexion before displacing the forearm of the specimen until failure at the elbow [6]. The native specimen could support a maximal valgus moment of 18.8±9.1 Nm before failure, which was characterized as ligament avulsion in 5 of 10 native specimens, and midsubstance rupture in 5 of 10 native specimens. The 30˚ flexion angle was chosen to open the olecranon from the surrounding bony fossa [[6], [7]]. Hechtman et al performed a similar test using the same flexion angle and obtained an ultimate valgus moment of 22.7±9.0 Nm. It was observed that there were significant discrepancies between results of paired left and right specimens. Failure in native UCLs were observed in the anterior band of the UCL only[7]. These observations indicate that repetitive loading on one limb or on one elbow may affect tolerance to valgus loading due to fatigue.
A cyclic test to failure indicated that the mean peak load to failure is 142.5±39.4 N, which translates to a mean peak valgus torque to failure of approximately 17.1 Nm based on the location of force application indicated in the test setup. The test was performed such that an initial 20N was applied for 200 cycles, after which the load is increased by 10N for another 200 cycles until there is observed complete ligament failure or a 5mm increase in ligament length. Failure in native ligament specimens was characterized as a disruption of ligament at the humeral attachment in 9 of 20 specimens, a disruption of ligament at the ulnar attachment in 4 of 20 specimens, and a disruption at midsubstance of the anterior bundle for 2 of 20 specimens. The remaining specimens saw failure via joint gapping[8].
Summarized results of the aforementioned cadaver UCL testing is shown in Table 2. These results indicate that cyclic loading indeed lowers the valgus loading threshold of the UCL by a considerable amount. There is also noticeable discrepancy between results of two similar cadaver tests, which can be attributed to differences in method of testing or cadaveric differences.
| Source | Type of Loading and Flexion Angle | Maximum Valgus Loading on UCL | Failures Observed |
|---|---|---|---|
| [6] | Ultimate, 30˚ | 18.8±2.1 Nm | Ligament avulsion and midsubstance disruption |
| [7] | Ultimate, 30˚ | 22.7±9.0 Nm | Disruption of anterior band |
| [8] | Cyclic, 90˚ | 17.1 Nm | Disruption of ligament at various points, joint gapping |
The UCL is also a major contributor to rotational stability and joint laxity of the elbow, which was observed in joint gapping failures in Table 2. In particular, the anterior band engages throughout extension and some flexion of the elbow (60˚ to 120˚ joint angle), whereas the posterior band engages in flexion only (0˚ to 60˚ joint angle). Based on cadaver testing, both bands are engaged at 60˚ flexion, which is the optimal angle to minimize ligament damage[9]. Human volunteer testing has indicated a 95˚ elbow flexion occurs during the first critical instant (arm cocking), and a 25˚ elbow flexion occurs during the second critical instant (deceleration) of a baseball pitch[5]. At these points, the UCL is especially vulnerable to failure as only one of the two bands are bearing the brunt of the elevated valgus torque.
Joint laxity was determined in cadaver testing by measuring the change in valgus angle of fiducial markers on the humerus and ulna at different flexion angles for an intact UCL and a transected UCL. In particular, Mihata et al tested joint laxity at 0˚, 30˚, 60˚, and 90˚ of elbow flexion to simulate the late cocking to acceleration phase of a baseball pitch[10]. Other aspects of the upper extremity, such as shoulder abduction, forearm pronation, and wrist extension, were controlled to mimic a typical baseball pitch. At all elbow flexion angles, elbow valgus laxity increases significantly after transection of the UCL, which is a strong indicator that the UCL is critical in providing rotational stability to the elbow[10]. Mihata also measured ulnar nerve strain by suturing 7 fiducial beads along the ulnar nerve at 1cm intervals. The change in bead distance after flexion testing indicates that ulnar nerve length increases exponentially at 60˚ and 90˚ flexion angles[10]. The findings from this cadaver test indicate that existing UCL microstrains or injuries may negatively affect valgus stability and strain the ulnar nerve, causing pain, decreased accuracy, decreased velocity, and the numb or tingling sensation that baseball pitchers commonly associated with UCL injuries[2].
Overall, cadaveric testing is beneficial to understand the biomechanics of UCL failure as a result of motions of a baseball pitch. Unlike testing with human volunteers, cadaveric testing offers the ability to instrument invasively on the UCL ligament, humerus and ulna, and the ulnar nerve to understand failures related to ligament disruption, joint gapping, and nerve stretching. Cadaveric testing also provides the added bonus of testing fatigue UCL injury, which cannot be done through human volunteers. However, replicating the complex throwing motion in a repeatable manner is complicated and often not biofidelic. This is best represented by the discrepancy of maximum UCL valgus loading between different cadaveric studies available in literature, as well as the discrepancy of maximum UCL valgus loading between cadaveric studies and human volunteer testing.
It is worthwhile to note that human volunteer testing shows a maximum valgus loading of 34.6 Nm, which surpasses the maximum valgus loading observed in cadaver testing[5]. Since it was not reported that any human volunteer subject suffered UCL injury, there appears to be controversy between the injury threshold determined from cadaveric studies and the UCL load calculated in human volunteer testing. Future cadaveric UCL research should focus on rectifying this discrepancy in threshold loading values and actual occurrences of injury, and on determining the threshold values for the various specific types of UCL injury observed in existing studies. Understanding the threshold of different UCL injuries in baseball pitchers will not only aid in the development of better reconstruction methods, but will aid in the prevention of UCL injury by promoting better form and technique during pitching.
Computer Simulation Experiments
There are few significant published studies that use only computer simulations to study biomechanics of the UCL joint[11]. This may be due to the readily available supply of human volunteers, and the usually chronic nature of the injury. Interest in this type of UCL injury simulation may grow as biofidelity and sophistication of simulation software improves.
Computer simulations are used, however, to quantify forces on specific tendons and muscles of the UCL joint based on human-volunteer videos. Elbow joint force simulation is difficult, because the contributions of activated non-UCL muscles and tendons are often unclear. The flexor digitorum superficialis muscle, for example, has been shown to significantly reduce load on the UCL joint during throwing[11]. This form of simulation is important because electromyographic (EMG) data collected from human volunteers has shown near-100% activation of multiple muscles during a pitch[11]. Non-biofidelic simulations of the UCL which don’t account for stabilizing muscle activations would therefore significantly overestimate the chance of UCL injury.
Another application of computer simulations in UCL injury research is using epidemiological information to create machine learning models of injury risk. This is possible because Baseball is a statistic-heavy sport, and databases for UCL injuries, throwing speeds, weather, game frequencies, and many other factors are available for research purposes (especially from the MLB)[12]. In one study, pitch variability has been shown to be a major risk-factor of UCL injury[12], suggesting that consistent-speed pitching may be important for injury reduction. Another key finding in this area is that the frequency of pitches thrown during a game is closely related to UCL injury risk, due to fatigue loading on the UCL joint[12]. This form of computer simulation modelling is uniquely suited to chronic forms of UCL injury.
Conclusion
UCL injuries in baseball pitchers are becoming increasingly prevalent as players exert more load on their arms in an effort to increase pitch velocity. Epidemiological data reinforces the need to assess this potentially preventable injury with research. Several biomechanical approaches have achieved results to help understand the injury modes: Human volunteer testing has provided data for how much load is typically exerted to the UCL complex. Cadaveric testing has identified the ultimate loading thresholds for varying failure modes, as well as the consequence of UCL injury to joint gapping and ulnar nerve strain. However, the limitations associated with measuring UCL force for human volunteer testing, as well as limitations to experimental setup and instrumentation for cadaveric studies, has led to significant discrepancy between the calculated UCL load in pitching and the expected injury threshold. Future work in this field includes rectifying this discrepancy to determine a reasonable ballpark injury threshold, the assessment of the injury mechanisms using finite element computer modeling methods, and additional research using cadaveric and human volunteer methods.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 J. R. Lynch, T. Waitayawinyu, D. P. Hanel, T. E. Trumble, “Medial Collateral Ligament Injury in the Overhand-Throwing Athlete”, The Journal of Hand Surgery, vol. 33, no. 9, pp. 430-437, 2008
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 J. R. Labott, W. R. Aibinder, J. S. Dines, C. L. Camp, “Understanding the medial ulnar collateral ligament of the elbow: Review of native ligament anatomy and function”, World Journal of Orthopedics. Vol 9, No. 6, pp. 78–84, 2018
- ↑ 3.0 3.1 M. W. L. Sonne and P. J. Keir, “Major League Baseball pace-of-play rules and their influence on predicted muscle fatigue during simulated baseball games,” Journal of Sports Sciences, vol. 34, no. 21, pp. 2054–2062, 2016.
- ↑ N. Y. Li, A. D. Goodman, N. J. Lemme, B. D. Owens, “Epidemiology of Elbow Ulnar Collateral Ligament Injuries in Throwing Versus Contact Athletes of the National Collegiate Athletic Association: Analysis of the 2009-2010 to 2013-2014 Seasons”, Orthopaedic Journal of Sports Medicine, VOL. 7, no. 4, 2019.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 G. S. Fleisig, J. R. Andrews, C. J. Dillman, and R. F. Escamilla, “Kinetics of Baseball Pitching with Implications About Injury Mechanisms,” The American Journal of Sports Medicine, vol. 23, no. 2, pp. 233–239, 1995.
- ↑ 6.0 6.1 6.2 G. A. Paletta , S. J. Klepps, G. S. Difelice, T. Allen, M. D. Brodt, M. E. Burns, M. J. Silva, and R. W. Wright, “Biomechanical Evaluation of 2 Techniques for Ulnar Collateral Ligament Reconstruction of the Elbow,” The American Journal of Sports Medicine, vol. 34, no. 10, Jun. 2000.
- ↑ 7.0 7.1 7.2 K. S. Hechtman, E. W. Tjin-A-Tsoi, J. E. Zvijac, J. W. Uribe, and L. L. Latta, “Biomechanics of a Less Invasive Procedure for Reconstruction of the Ulnar Collateral Ligament of the Elbow,” The American Journal of Sports Medicine, vol. 26, no. 5, pp. 620–624, 1998.
- ↑ 8.0 8.1 A. D. Armstrong, C. E. Dunning, L. M. Ferreira, K. J. Faber, J. A. Johnson, and G. J. W. King, “A biomechanical comparison of four reconstruction techniques for the medial collateral ligament–deficient elbow,” Journal of Shoulder and Elbow Surgery, Mar. 2005.
- ↑ Y. Matsuura, T. Takamura, S. Sugiura, Y. Matsuyama, T. Suzuki, C. Mori, and S. Ohtori, “Evaluation of anterior oblique ligament tension at the elbow joint angle—a cadaver study,” Journal of Shoulder and Elbow Surgery, 2020.
- ↑ 10.0 10.1 10.2 T. Mihata, M. Akeda, M. Künzler, M. H. Mcgarry, M. Neo, and T. Q. Lee, “Ulnar collateral ligament insufficiency affects cubital tunnel syndrome during throwing motion: a cadaveric biomechanical study,” Journal of Shoulder and Elbow Surgery, vol. 28, no. 9, pp. 1758–1763, 2019.
- ↑ 11.0 11.1 11.2 Trigt, Bart van, Ton (AJR) Leenen, Marco (MJM) Hoozemans, Frans (FCT) van der Helm, and Dirkjan (HEJ) Veeger. “Are UCL Injuries a Matter of Bad Luck? The Role of Variability and Fatigue Quantified.” Proceedings 49, no. 1 (2020): 107.
- ↑ 12.0 12.1 12.2 Buffi, James H., Katie Werner, Tom Kepple, and Wendy M. Murray. “Computing Muscle, Ligament, and Osseous Contributions to the Elbow Varus Moment during Baseball Pitching.” Annals of Biomedical Engineering 43, no. 2 (February 2015): 404–15.