Documentation:FIB book/PCL Dashboard Impacts in Motor Vehicle Collisions
Summary
The posterior cruciate ligament (PCL) is one of four primary ligaments comprising the knee joint, attaching the posterior face of the tibia to the femur's medial condyle. The PCL acts as a joint stabilizer, protecting the knee from excessive posterior tibial translation and external rotation.[1] Direct blows to the knee compromise PCL integrity, particularly when the knee is in a flexed position. This mechanism is known as pretibial trauma and is most commonly seen in motor vehicle crashes (MVCs) where a bent knee strikes the dashboard (45% of PCL injuries).[2] Injury types from pretibial trauma vary by direction of impact, requiring conservative or operative treatment based on severity.
Commonly reported symptoms of PCL tear include knee stiffness, instability, and abnormal gait. Missed diagnoses are attributed to a lack of research and understanding of epidemiology. Our current understanding of PCL injury tolerances is from PMHS experiments, which have shown that PCL integrity is compromised via excessive tibial translation relative to the femur.
To date, a variety of engineered measures exist to reduce the risk of PCL injury in a frontal collision in modern motor vehicles. The main design consideration is to prevent the occupant from impacting the dashboard (i.e. FMVSS seat belt standards, seat location). However, there are also design considerations to the dashboard to aid in injury prevention.
Controversial engineered injury prevention strategies include knee airbags (KABs), designed to reduce risk of injury to the lower extremities. Recent studies contradict their purpose, as KABs were found to offer insignificant risk reduction for frontal collisions. Moreover, they may elevate risk of injury to regions below the knee, particularly the foot and ankle.
Background
Research has been mainly performed on topics of knee joint anatomy, PCL anatomy and function, epidemiology, and PCL tear treatment. This paper identifies a few weaknesses in the current literature surrounding PCL injuries. Specifically, there is a lack of research studying PCL injury biomechanics and further research is needed to validate the relationship between posterior tibial slope and risk of PCL injury; a lack of consensus exists surrounding both risk factors as well as the most appropriate graft and technique to be used in PCL reconstructive surgery; there is also no gold standard that currently exists for PCL rehabilitation.
Knee Joint Anatomy
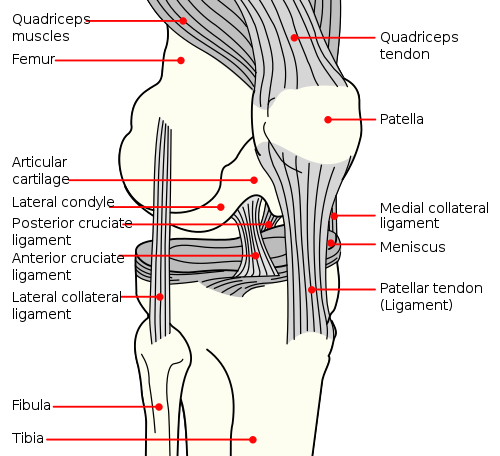
The knee is the largest joint in the human body, responsible for weight-bearing and movement.[3] The femur (thigh bone), tibia (shin bone), and patella (kneecap) are connected via four primary ligaments: the anterior cruciate ligament, posterior cruciate ligament, lateral collateral ligament, and medial collateral ligament. As seen in Figure 1, the collateral ligaments are situated on the sides of the knee, and cruciate ligaments are inside the knee joint.[1]
Posterior Cruciate Ligament Anatomy and Function
The posterior cruciate ligament connects the posterior face of the tibia to the femur's medial condyle (articular cartilage encapsulating the femur base). The PCL provides strength and stability, protecting the knee from excessive posterior tibial translation and external rotation moments.[4] PCL length ranges 32 to 38 mm, with an average cross-sectional area of 12 mm2; twice that of the ACL.[5] Ligament thickness is fundamental to its significant tensile strength, ranging from 739 to 1627 N depending on the direction of loading.[4][6] Two fibrous bundles comprise the PCL (anterolateral and posteromedial bundles), synergistically functioning to maintain appropriate ligament tension.[6] A PCL injury is when the PCL is torn or sprained and many events can cause PCL injuries.[7]
Epidemiology
PCL injuries result from direct impact to the knee joint, particularly when the knee is in a flexed position. This mechanism is most commonly seen in motor vehicle crashes (MVCs), where a bent knee hits the dashboard.[4] MVCs are the leading cause of PCL injury (45%), with the most common mechanism being dashboard injuries (35%).[8][9]
Obtaining PCL diagnosis in the early stages of injury continues to be an ongoing issue.[8] A 2003 observational study conducted by Schulz et al. found mean symptom duration to be 44.4 +/- 68.6 months at the time of assessment; only 10.3% of patients were seen within 30 days of injury. The average patient age was 27 years, with male patients constituting the majority of seen cases (79.4%).[9]
Due to the lack of research present for PCL injuries, there is no consensus on risk factors. Notably, recent biomechanical studies have associated a smaller posterior tibial slope to an increased risk of PCL injury.[10] Further clinical research is needed to evaluate how a decreased tibial slope impacts knee kinematics and stability, thus compromising the integrity of the PCL.
PCL Tear Treatment
Pain, intra-articular swelling, and joint tenderness are immediate symptoms of PCL tears, causing limited range of motion and difficulty walking. After swelling subsides, joint instability and stiffness are commonly felt during activities of daily living, ultimately compromising one’s quality of life.[11]
Three grades exist for classifying PCL injuries: Grade I (partial tear), Grade II (complete isolated tear), and Grade III (complete PCL tear with combined capsular and/or ligament injury).[11] Diagnosis requires physical examination from a clinician and medical imaging (i.e. MRI). Depending on tear severity, conservative and surgical treatment options are available. Conservative approaches work under the guidance of a physical therapist, targeting bracing, quadricep strengthening, and recovery of proprioception to promote spontaneous healing of the ligament.[8][12][13] Operative treatment is typically reserved for those with Grade III tears and high functional demands, following ineffective conservative treatment.[11][14] Due to the infrequent nature of PCL surgical intervention, there is little consensus on the most appropriate graft type and technique for reconstructive methods.[15] Furthermore, there is no “gold-standard” rehabilitation protocol. Typically, full recovery requires six to twelve months of rehabilitation under the guidance of a physical therapist and orthopedic surgeon. Such rehabilitation programs generally target restoring range of motion and strength through a progression of bracing, weight-bearing, and quadricep strengthening.[16]
While the ACL is more frequently injured, PCL injuries can have significant consequences if left unmanaged.[8][11] Proper diagnosis, treatment, and rehabilitation are fundamental to regaining knee function and preventing disruption to quality of life. Understanding PCL injury mechanisms and implementing injury prevention strategies are essential to improving the quality of care.
Injury Mechanisms of PCL Injuries
Pretibial Trauma as a Mechanism of PCL Injury
The significant mechanism of how the PCL is often injured in dashboard panel impacts is known as pretibial trauma. This occurs because, in these accidents, the knee is often bent, and a force is directed towards the front part of the knee. The mechanism of pretibial trauma involves applying a direct force to the proximal anterior tibia, and this results in specific patterns of knee injury, described below.[17]
There are various types of PCL injuries caused by pretibial trauma. For example, one type is intrasubstance tears, which are tears within the PCL itself. Intrasubstance tears occur at the tibial plateau (i.e., the flat, top surface of tibia bone), or as tibial avulsions, where the PCL detaches from the tibia. In the cases of more serious MVCs, higher dashboard impact forces can also harm subsequent knee anatomy such as the meniscofemoral ligaments, signifying a Grade III PCL tear.[17]
Furthermore, the direction of the force from the dashboard influences the specific type of PCL injury. If the impact force pushes towards the front of the tibia and involves a twisting motion, it can damage the posterolateral corner. This is a complex area of ligaments and tendons on the anterior and lateral side of the knee joint, crucial for knee stabilization and movement control. In cases where the knee is forced into extension (i.e. straightening the leg) upon impact with the dashboard, a part of the PCL tightens and might detach from its attachment point.[17]
Patients who experience PCL injuries due to pretibial trauma often have increased knee instability compared to PCL injuries obtained from other mechanisms, such as hyperflexion (i.e., excessive extension of the knee). Understanding this injury mechanism is crucial for determining the most effective treatment option, which can range from non-operative approaches for partial or isolated PCL injuries (Grades I and II) to surgical interventions for non-isolated complete tears (Grade III).[17]
Injury Tolerance of PCL During Dashboard Panel Impacts
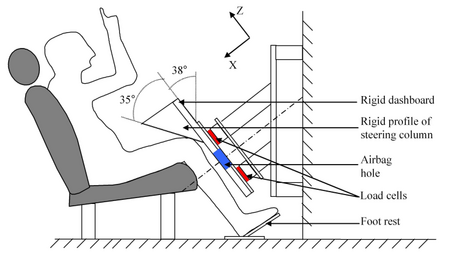
To understand the injury limits of the PCL during dashboard impacts, several studies have conducted experiments using Post Mortem Human Surrogates (PMHS). The test set-up is shown in Figure 2.[18] The aim of these studies was to indirectly measure injury tolerance of the PCL by estimating the injury threshold of the tibial drawer. The tibial drawer measurement is used to identify PCL injury in these studies because the tibia pulling away from the femur can lead to injuring the PCL, and the injury mechanism matches that of dashboard panel impacts.[18]
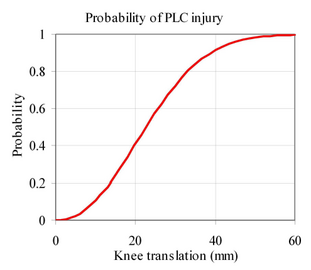
In these studies, researchers including Viano et al.,[19] Balasubramanian et al.,[20] and Meyer et al.,[21] found that PCL damage usually happens when there is an average tibial translation of 16 mm relative to the femur. Average translation was calculated following trials with multiple PMHS specimens, ranging from 9.5 to 30 mm of tibia translation.[18]
Leport et al. used the data from these studies and others in the literature to create an injury risk curve for the PCL (Figure 3).[18] The curve shows the probability risk of PCL injury (%) in comparison to displacement of the tibia (mm). Note that survival analysis techniques were applied to determine the curve (statistical concept that allows for estimating the probability of the injury over time). This information can help researchers and clinicians to understand the likelihood of PCL injuries based on testing and observing the tibia’s movement in those who have experienced MVCs. Additionally, this information aids in the development of injury prevention strategies and measures.[18]
Design for Injury Prevention
To date, there are a variety of designed measures to reduce the risk of PCL injury from a frontal collision in a modern motor vehicle. The primary consideration is to prevent the occupant from impacting the dashboard. Subsequently, there are also dashboard design considerations which can prevent injury. The standards set by the Federal Motor Vehicle Safety Standards (FMVSS) carry influence, yet there are further measures taken by automotive manufacturers, such as additional airbags, dashboard design, and seat positioning.
Seatbelt and Seat Considerations
Federal Motor Vehicle Safety Standard 208 (FMVSS 208) focuses on occupant crash protection, sets the regulations for seatbelts and airbags to safeguard the occupants during a collision. In the case of a frontal collision, the seatbelt plays a critical role in preventing the occupant from coming in contact with the dashboard. FMVSS 208 specifies that it should be a three-point belt with lap and shoulder restraints. It also specifies factors such as strength, durability, and capacity to effectively secure occupants during a collision. Beyond the belt itself, FMVSS 208 specifies belt attachment points in the vehicle structure, to ensure the occupant is effectively restrained. More recently, this has included specifications requiring the upper attachment point of the shoulder belt to be adjustable to accommodate varying sized occupants. Furthermore, the seat belt must have an automatic pretensioner so that the seat belt tightens in the case of a crash or rapid deceleration, preventing the occupant from sliding forward towards the dashboard.
Car seat positioning also plays an important role in the likelihood of dashboard impact upon MVC. The further away the occupants' knees are from the dashboard or steering wheel, the less likely the occupant is to experience an impact force significant enough for PCL injury.[18] The vertical position of the seat also impacts occupant safety, as the force required to displace the tibia relative to the femur depends on the height of impact to the tibia. Moreover, a higher amount of force is required to create the same displacement as the contact point moves towards the ankle.[22] Notably, FMVSS does not consider the position of the car seat relative to the dashboard or the floor. Instead, this is set by the manufacturer to determine a safe range of operation.
Airbag Considerations
Airbags play a crucial role in protecting the occupants of MVCs. FMVSS 208 specifies requirements for a variety of airbags including driver, front passenger, side, and curtain. The driver and the front passenger airbag standards found in FMVSS 208 hold the highest significance for decelerating the occupants of MVCs in frontal collisions. Despite this, they have little effect on PCL injuries.
Knee airbags (KABs) have been suggested as a measure to reduce the force of impact of the occupant’s knees on the dashboard. They are often implemented on the driver's side, and have been shown to reduce the impact force by 15-20%.[23] However, in the case where vehicle occupants are out of position (i.e. with their knees touching the dashboard), a knee airbag can have adverse effects and increase the force experienced by the occupant.[18] KABS have been shown to increase lateral knee displacement and abduction angle for occupations that are out of position. This can cause increased loading of the tibia which can cause PCL injuries despite KAB deployment.[24]
Optimization of dashboard profile and stiffness at key contact locations is pivotal in the goal of PCL injury prevention. For passengers, the design of the glove box specifically, plays a critical role in PCL injuries. In the case of a frontal collision where the knees impact the dashboard, the femur base will penetrate into the dashboard through the glovebox, while the tibia will stop at the lower edge of the dashboard. This will cause excessive tibial translation, resulting in a PCL injury. This effect can be avoided by increasing the glovebox stiffness to prevent knee penetration into the dashboard, through the glovebox. Additionally, the stiffness of the dashboard can be lowered where the tibia is expected to impact. This can be done either by material selection or with geometric weakening.[22]
Dashboard Considerations
Optimization of dashboard profile and stiffness at key contact locations is pivotal in the goal of PCL injury prevention. For passengers, the design of the glove box specifically, plays a critical role in PCL injuries. In the case of a frontal collision where the knees impact the dashboard, the femur base will penetrate into the dashboard through the glovebox, while the tibia will stop at the lower edge of the dashboard. This will cause excessive tibial translation, resulting in a PCL injury. This effect can be avoided by increasing the glovebox stiffness to prevent knee penetration into the dashboard, through the glovebox. Additionally, the stiffness of the dashboard can be lowered where the tibia is expected to impact. This can be done either by material selection or with geometric weakening.[22]
Problems, Controversies, and Limitations
Studies on PCL injury reconstruction in dashboard injuries are scarce, this results in a lack of understanding of the biomechanics behind them. However, there are a few studies that have been conducted on the interaction of knee injuries with KABs. Problems and limitations are drawn but controversies are not discovered in our research.
A study by McMurry et al. found that KABs have reduced the risk of injuries to the lower extremities. However, there may be an increase in injuries to the area below the knee, particularly the foot and ankle. Although these injuries are not life-threatening, they severely impact long-term mobility and quality of life.[25][26] Additionally, they predominantly affect women, accounting for 78% of lower extremity injuries upon KAB deployment. The exact cause of these injuries and their relationship to KAB deployment are not fully understood and require further research. Although knee-specific injuries appear frequent when KABs are deployed, it is unclear if the increase in below-knee injuries is a direct result of the KAB deployment or additional factors.[27]
Consistently, drawing on frontal crash test data from the Insurance Institute for Highway Safety (IIHS) and police-reported crash data across 14 states, it is established that KABs offer no significant reduction in injury risks during frontal collisions, regardless of test type (controlled or actual). In fact, they may elevate injury risk to the upper and lower tibia, foot, and femur. Furthermore, after accounting for variables such as vehicle weight, model year, and driver characteristics, KABs still do not show a significant reduction in overall injury risk. Conclusively, the research suggests that the efficacy of KABs in enhancing passenger safety is questionable and their potential adverse effects should lead manufacturers to reassess KAB inclusion in future motor vehicles.[28]
Future Research
Current studies do not provide a clear understanding of the mechanisms of PCL injuries or injury tolerances. To obtain tolerances, current methods only measure indirectly how far the tibia translates, rather than measuring the direct forces and stresses applied to the PCL during panel impacts. Future research should integrate direct measurement techniques to assess the stresses and strains of the PCL in PMHS testing to deepen our understanding of PCL injury mechanics and tolerances. Furthermore, it is important to expand PMHS sample sizes to include pediatric and other underrepresented populations. Additionally, further work is needed to reduce the subjectivity inherent in PCL injury diagnoses via tibial drawer measurements, and efforts are required in using Accident Reconstruction findings to understand the injury tolerances. With a better understanding of PCL injury mechanisms and tolerances, safer and more impactful injury prevention strategies can be developed, especially around KABs.
Simultaneously, it is important to advance the evaluation of knee airbag (KAB) efficacy in static deployment scenarios. While current research offers some insights, prospective research must aim to identify accurate, predictive metrics for injury risk. To date, limited research has been conducted on the real-world effectiveness of KABs, biofidelity of crash test dummies, and methodologies for predicting injuries in static deployments. Thus, a focused research initiative should begin with comparative testing using human cadaver models alongside crash test dummies to investigate injury patterns, associated risk factors, and the validity of dummy metrics in forecasting injury risks. This research approach is pivotal for developing safer vehicle systems and protective measures against PCL injuries in frontal collisions.[27] With a clearer understanding of injury metrics, crash test dummies can be more representative and better validate safety designs around PCL injuries in MVCs.
References
- ↑ 1.0 1.1 "Posterior Cruciate Ligament Injuries". OrthoInfo - AAOS.
- ↑ "Posterior Cruciate Ligament (PCL) Injury". HealthLink BC.
- ↑ Pache, Santiago; Aman, Zachary; Kennedy, Mitchell; Yoshinobu Nakama, Gilberto; Moatshe, Gilbert; Ziegler, Connor; LaPrade, Robert (January 2018). "Posterior Cruciate Ligament: Current Concepts Review". Arch Bone Jt Surg. 6: 8–18.
- ↑ 4.0 4.1 4.2 Logterman, Stephanie; Wydra, Frank; Frank, Rachel (May 31, 2017). "Posterior Cruciate Ligament: Anatomy and Biomechanics". Curr Rev Musculoskelet Med. 11: 510–514.
- ↑ Girgus, F; Marshall, J; Monajem, A (February 1975). "The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis". Clin Orthop Relat Res. 106: 216–231.
- ↑ 6.0 6.1 Butler, D; Kay, M; Stouffer, D (1986). "Comparison of material properties in fascicle-bone units from human patellar tendon and knee ligaments". J Biomech. 19: 425–32.
- ↑ "Posterior Cruciate Ligament (PCL) Injury: Symptoms & Treatment". Cleveland Clinic.
- ↑ 8.0 8.1 8.2 8.3 Lee, Beom; Nam, Shin (September 2011). "Rupture of Posterior Cruciate Ligament: Diagnosis and Treatment Principles". Knee Surg Relat Res. 23: 135–141.
- ↑ 9.0 9.1 Schulz, M; Russe, K; Weiler, A; Eichhorn, H; Strobel, M (May 2003). "Epidemiology of posterior cruciate ligament injuries". Arch Orthop Trauma Surg. 123: 186–91.
- ↑ Bernhardson, Andrew; DePhillipo, Nicholas; Daney, Blake; Kennedy, Mitchell; Aman, Zachary; LaPrade, Robert (February 2019). "Posterior Tibial Slope and Risk of Posterior Cruciate Ligament Injury". Am J Sports Med. 47: 312–17.
- ↑ 11.0 11.1 11.2 11.3 Raj, Marc; Mabrouk, Ahmed; Varacallo, Matthew (2023). Posterior Cruciate Ligament Knee Injuries. StatPearls Publishing.
- ↑ Lopez-Vidriero, E; Simon, DA; Johnson, DH (December 2010). "Initial evaluation of posterior cruciate ligament injuries: history, physical examination, imaging studies, surgical and nonsurgical indications". Sports Medicine and Arthroscopy Review. 18: 230–237.
- ↑ Matava, Matthew; Ellis, Evan; Gruber, Brian (July 2009). "Surgical treatment of posterior cruciate ligament tears: an evolving technique". J Am Acad Orthop Surg. 17: 435–46.
- ↑ Vandenrijt, Jasper; Callenaere, Sofie; Van der Auwera, Dries; Michielsen, Jozef; Van Dyck, Pieter; Heusdens, Christiaan (2023). "Posterior cruciate ligament repair seems safe with low failure rates but more high level evidence is needed: a systematic review". Journal of Experimental Orthopaedics. 10: 49.
- ↑ Montgomery, Scott; Johnson, Jared; McAllister, David; Petrigliano, Frank (June 2013). "Surgical management of PCL injuries: indications, techniques, and outcomes". Curr Rev Musculoskelet Med. 6: 115–23.
- ↑ Fanelli, Gregory (February 2008). "Posterior cruciate ligament rehabilitation: how slow should we go?". Arthroscopy. 24: 234–5.
- ↑ 17.0 17.1 17.2 17.3 Janousek, A; Jones, D; Clatworthy, M; Higgins, L; Fu, F (December 1999). "Posterior cruciate ligament injuries of the knee joint". Sports Med. 28: 429–41.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 Leport, Tiphaine; Baudrit, Pascal; Petit, Philippe; Trosseille, Xavier; Vallancien, Guy (2008). "Evaluation of the risk of injury caused by a knee airbag in out-of-position" (PDF). National Highway Traffic Safety Administration (NHTSA): 1–7.
- ↑ Viano, David; Culver, Clyde; Haut, Roger; Melvin, John; Bender, Max; Culver, Roger; Levine, Robert (1978). "Bolster Impacts to the Knee and Tibia of Human Cadavers and an Anthropomorphic Dummy". SAE International: 1–11.
- ↑ Balasubramanian, Sriram; Beillas, Philippe; Belwadi, Aditya; Hardy, Warren; Yang, King; King, Albert; Masuda, Mitsutoshi (November 2004). "Below Knee Impact Responses using Cadaveric Specimens". Stapp Car Crash J. 48: 71–88.
- ↑ Meyer, Eric; Sinnott, Michael; Haut, Roger; Jayaraman, Gopal; Smith, Walter (November 2004). "The Effect of Axial Load in the Tibia on the Response of the 90 degrees Flexed Knee to Blunt Impacts with a Deformable Interface". Stapp Car Crash J. 48: 53–70.
- ↑ 22.0 22.1 22.2 Gokhale, Ajit; Saravate, Vithoba; Kshirsagar, Sarang (2009). "Dashboard Stiffness Control for Reducing Knee Injury in Frontal Crashes". SAE International: 1–5.
- ↑ Makwana, Rahul; Jindal, Pardeep (2019). "Innovative Knee Airbag (KAB) Concept for Small Overlap and Oblique Frontal Impacts". SAE International: 1–7.
- ↑ Nie, Bingbing; Crandall, Jeff; Panzer, Matthew (February 2017). "Computational investigation of the effects of knee airbag design on the interaction with occupant lower extremity in frontal and oblique impacts". Traffic Inj Prev. 18: 207–215.
- ↑ Dischinger, PC; Read, KM; Kufera, JA; Kerns, TJ; Burch, CA; Jawed, N; Ho, SM; Burgess, AR (2004). "Consequences and costs of lower extremity injuries". Annu Proc Assoc Adv Automot Med. 48: 339–53.
- ↑ McMurry, Timothy; Sherwood, Chris; Poplin, Gerald; Seguí-Gómez, María; Crandall, Jeff (2015). "Implications of Functional Capacity Loss and Fatality for Vehicle Safety Prioritization". Traffic Inj Prev. 16: 140–5.
- ↑ 27.0 27.1 McMurry, Timothy; Forman, Jason; Shaw, Greg; Crandall, Jeff (2020). "Evaluating the influence of knee airbags on lower limb and whole-body injury". Traffic Inj Prev. 21: 72–77.
- ↑ Monfort, Samuel; Mueller, Becky (July 2019). "Effectiveness of knee airbags across two crash paradigms". Insurance Institute for Highway Safety: 1–20.