Documentation:FIB book/A scoping review on facial ATDs
The field of injury biomechanics has historically focused on preventing severe and fatal injuries. This is demonstrated by the development of anthropometric test devices (ATDs), whose primary intent is to create biofidelic responses for the major body areas, such as the head, neck, chest, and knees[1]. However, survivors of traumatic facial injuries often suffer from psychological distress, altered social lifestyles, and a reduced quality of life[2]. Facial injuries can result in irreversible damage to organs located on the face, such as the eyes and the nose. Nasal injuries, in particular, are among the most common facial injuries and can lead to serious complications such as septal hematoma, septum necrosis, and permanent nose deformity[3]. Consequently, patients may experience difficulties in breathing through the nose or suffer from unpleasant odors emanating from it[4].
Currently, there is a significant research gap in the biomechanical study of facial injuries in the context of ATDs. The limited avenues for studying and characterizing facial injuries in a biomechanical setting highlight the need for reviewing the current literature on the various transducers and techniques used in injury biomechanics to assess facial injury risk. With this knowledge, future research can be done to better understand facial injuries along with their prevention and advance the field of ATDs.
While facial injuries may not commonly reach a level of severity that poses a direct threat to life, they are a significant concern due to the quality-of-life implications caused by facial damage. This review will thoroughly examine the prevalence and occurrence of facial injuries in the context of car accidents, providing essential background information. Following this, a detailed exploration of the mechanical properties of facial bones and soft tissue will be conducted to understand how these structures respond and change under impact scenarios. The primary focus of the review lies in the chronological analysis of the development of trauma-indicating and trauma-sensing ATD headforms, and of how they detect facial injuries.
Ultimately, this literature review aims to provide a holistic summary of facial injury in the context of ATDs and current biomechanics-based methods for analyzing such impacts to fill the existing research gap while contributing valuable insights into the biomechanics of facial injuries and their prevention.
Background
In order to thoroughly understand the needs of facial ATDs, one must first acquire insight into the anatomy and injury tolerances of the face and common facial injuries resulting from motor vehicle accidents (MVAs). A study featured in The Journal of Craniofacial Surgery found that (MVAs) were a leading cause of maxillofacial injuries (face and jaw injuries)[5]. Of the facial injuries caused by MVAs in the study, only about 50% of patients sustained open wounds such as lacerations, abrasions and burns[5]. However, 80% of the patients suffered facial bone fractures with the nasal bones being the most frequent region of fracture, followed by the zygomatic bones (cheekbones)[5]. Though less frequent in comparison, fractures to the maxilla and frontal were also reported in MVAs[5] [6] [7].
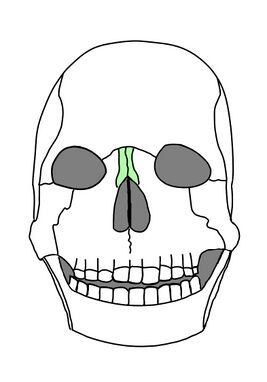
Nasal Bones
The nasal bones, shown in Figure 1, are two small bones located symmetrically in the midface in between the two eye sockets, and play a role in forming the bridge of the nose[8].
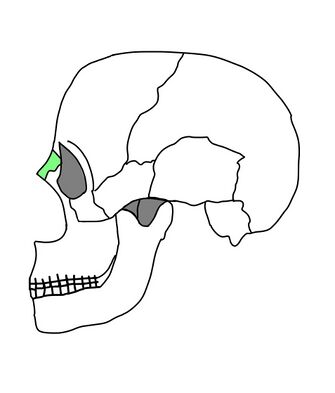
In a sagittal plane view, the nasal bones protrude slightly as depicted in Figure 2, making them a point of initial contact in an impact to the face. Blunt forces to the nasal bones ranging from 450 N to 850 N are associated with a 50% risk of fracture, while more severe fracture patterns require forces approaching 3000 N, which would be equivalent to bearing a 672.4 lb weight on your height[9][3]. An explanation for this large range of forces can be attributed to the prominent, pointed tip of the nasal bones. If a load is applied directly onto the tip, then there will be significant stress concentrations exerted onto the bone, requiring less force to induce a fracture. Conversely, if a load is applied to the flat "bridge" of the nasal bones, there will be greater force distribution along the entirety of the bones and thus reduce the likelihood of a fracture.
.
Zygomatic Bones
The zygomatic bones, otherwise known as the cheekbones, are a pair of bones situated on the anterior and lateral regions of the face as illustrated in Figure 3. They function in bearing the load of mastication and forming the prominence of the cheeks[4]. As with the nasal bones, the zygomatic bones are susceptible to injury due to their prominence, but can withstand up to about 4450 N[10].
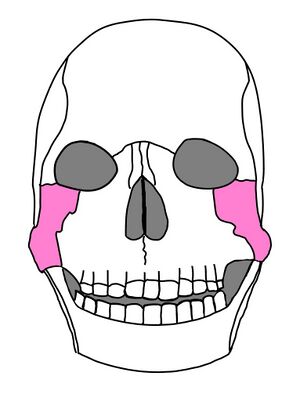
Maxilla
The maxilla is located at the center of the midface and surrounds the nasal bones, as depicted in Figure 4. In addition to forming the upper jaw, it also separates the nasal and oral cavities[11]. In comparison to the other facial bones, the maxilla exhibits a slightly thinner wall, and thus can only withstand up to about 1980 N of force before fracture[12].

Frontal Bone
Finally, the frontal bone (detailed in Figure 5) is the large bone that makes up the forehead and brow ridges, and its main purpose is to protect the frontal lobe[13]. As a result of having such an important role, the frontal bone exhibits the highest fracture threshold of up to 7100 N due to its large surface area (greater force distribution)[12].

Summary of Previous Work
Melvin et al.’s first dummy (1969)
In 1969, Melvin et al. published a seminal paper on the development of a frangible ATD headform that indicated facial injury[12]. Their goal was to create a frangible skull that would be biofidelic in localized penetration impacts when impacted with surfaces smaller than 1 square inch. Until this point, the only facial ATDs were laceration-indicating headforms with an artificial soft layer wrapped over a standard ATD head such as the VIP Series. Laceration headforms aimed to replicate skin and soft tissue injury and they were motivated by the fact that advancements in the windshield industry were leading to more superficial lacerations[14].
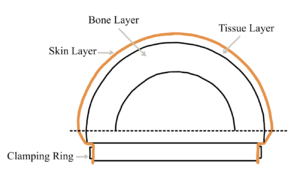
To address the lack of trauma-indicating headforms, Melvin et al. created a headform consisting of an aluminum backing plate, a simulated skull cap made of foamed ABS plastic, a simulated subcutaneous tissue layer made of a natural rubber material, and a synthetic skin layer (Figure 6). In steel cylindrical penetrator impact tests on cadaver skulls, the authors observed that the skull penetration profile is highly localized when using small impactors, and also that the frontal bone is twice as resistant to penetration compared to the parietal bone. Therefore, they opted to use a 31 lb density ABS plastic crushed to 10% of its original thickness to represent the frontal bone, and a 20.5 lb density ABS plastic crushed to 20% of its original thickness to represent the parietal bone. These material and crush value choices were determined from the embalmed cadaver impact tests but the authors acknowledged that the force-deflection values of their cadaver tests may be inaccurate due to the embalmed and elderly state of their small sample size.
It is noteworthy that Melvin et al. considered creating a segmented load-sensing headform but decided against it because of the challenges of instrumentation. They also suggested that it was not necessary to create a headform that would sense loads in segmented regions of the face for >1 sq. in. impacts because the magnitude at which these impacts would cause skull fracture would probably be the same magnitude that would cause brain injury. They followed this by saying that large-surface-area impacts could rather be measured with a standard head accelerometer in existing ATDs. This perhaps hinted that the purpose of their headform was purely to prevent fatal injuries rather than to reduce facial damage for quality-of-life purposes. Nonetheless, their work was the first of its kind and it paved the way for the future development of other trauma-indicating headforms.
Tarrière et al.’s Biomechanical Model of the Human Face (1981)

In 1981, Tarrière et al. analyzed data from Le Laboratoire de Physiologie et de Biomécanique Peugeot S.A./Renault and determined that that the face is the most common area of injury during severe motor vehicle accidents, and that ATDs at the time failed to accurately model human faces. As such, his team conducted research into better understanding human facial features in order to design a more realistic ‘face’ that is detachable and adaptable to the heads of dummies at the time. Through extensive testing, they determined RTV 1502 silicon to be the most appropriate model of human skin based on factors such as mechanical properties, stability and potential of adherence to plastic foam that simulated adipose tissue[15]. They also conducted various tests to thoroughly understand the mechanical properties of the facial bones and concluded that the honeycomb material AMI 4-40 was the best representative material[15]. With each material determined, the team then assembled their face model by gluing the honeycomb material onto a fine metal plate, then screwing it to a metal support (AS-13 aluminum-alloy) that was welded to a Hybrid II dummy (HII) skull (Figure 7)[15]. Next, the simulated soft tissue and adipose tissue was placed on top, and clamped to the head on the skull’s sides. This model of the human face was ultimately designed to allow researchers to study the facial injuries associated with impacts to the steering wheels, windshields and other objects in the vehicle during tests. By conducting the same experiments on their model and human cadaver faces, they concluded that their model accurately simulates the characteristics of laceration, facial resistance and energy-absorption capacity of the human face. Their model also facilitated repeatable tests due to the interchangeability of the various materials, and introduced the ability to gauge the degree of impact without measuring devices by analyzing the degree of deformation of the model. Though this study was conducted several decades ago, it provides great insight into facial ATDs that accurately stimulate soft tissue injuries without requiring the use of PMHS, which can become resource-heavy over time.
Warner et al.’s Biomechanical Face for the Hybrid II (1986)
Whereas Melvin et al. argued that a frangible headform is preferable over a segmented, load-sensing faceform[12], Warner et al. countered this by pointing out that frangible faceforms lack repeatability (because of their one-time use) and force-time history data[16]. In 1986, Warner et al. took on a unique approach compared to previous facial ATDs by adapting the existing Hybrid II head and adding a pressure sensing film over the face. From recent biomechanical data on facial injury tolerances[17][18], they recognized the need for a multi-segmented face because facial bony load limits are different for the different regions of the face. They also recognized that facial injuries, while usually not high on the AIS scale, often decrease long-term quality of life, and that the existing accelerometer in the Hybrid II head could not predict specific facial injuries.
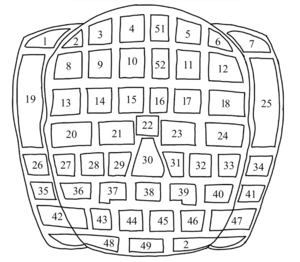
Their device consisted of 52 piezoelectric plastic films, shown in Figure 8, that were attached to the flat surfaces of the aluminum Hybrid II face. The original synthetic tissue and skin layers were then put over top the sensors. Each sensor had a cable that was directed to the center of the ATD skull where it was connected to a central data acquisition and storage system. Room was kept inside the skull for the existing accelerometer. Preliminary validation of the pressure-sensing film was done by impacting the face with a styrofoam-padded impactor and comparing the sensor outputs with the output of calibrated strain gauge pressure transducers. Although the sensors passed the tests, Warner et al. did not conduct any tests in a vehicle collision facial impact scenario, so there was no guarantee that the sensors were accurate in a real crash. Another limitation of their design was that the bulkiness of the instrumentation was potentially affecting the head’s inertial and kinematic properties which decreased biofidelity [14][16]. Nonetheless, Warner et al. created a novel way to measure localized facial pressures on existing ATDs such as the Hybrid II, and they were recognized as such by future researchers in the field[13].
General Motors Hybrid III Deformable Face (1989)
In 1989, Melvin and Shee developed an adapted Hybrid III head with deformable facial characteristics, and in 1995, Melvin et al. published a paper outlining the development of the 1989 dummy [13]. The authors aimed to create a culmination of the previous work in trauma-indicating faceforms. Similar to Warner et al.'s 1986[16] and Tarriere et al.’s 1981[15] devices, they wanted to create an adaptation to an existing ATD for ease of implementation. However, unlike the 1986 headform, they wanted to ensure that any additional instrumentation in the head does not alter the inertial and kinematic properties of the head. Also, whereas some previous devices focused only on distributed loading[15] and some only on localized loading[12], Melvin and Shee intended to create a headform that was accurate for both distributed and localized loading. This decision was justified by biomechanical data published in the 1980s which highlighted that localized and distributed loading can both cause facial fractures and that they each have unique load responses[3][15][19].
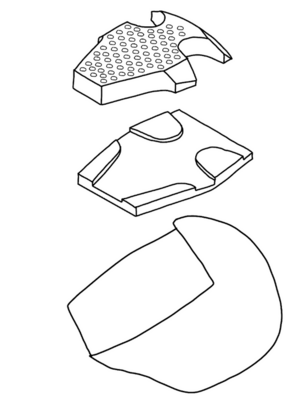
Melvin and Shee cut away a section of the Hybrid III face and placed a frangible insert made of rubber and high density polystyrene foam with varying thicknesses and a hole pattern to recreate the force-deflection characteristics of different regions of the face (Figure 9). No holes were drilled in the area above the eyes because there was no force-deflection data available for that facial region at the time. They also turned away from the localized force sensors of Warner et al.’s 1986 headform and instead created a mathematical program to find the magnitude and location of the impact force. They did so by applying Newton's Laws and considering the balance of inertial forces and neck reaction forces. The approach utilized the known shape of the head and the assumption that the early-phase head motion after impact was planar motion.
The Hybrid III deformable face was perhaps the most extensively validated headform of its kind, and it was validated by recreating facial injury tolerance tests conducted in the same decade[3][19]. The first series of tests were with varying diameter impactors, and these resulted in force-deflection and force-time curves that fit the biomechanical corridors for both localized and distributed loading. The second series of tests were sled tests comparing the standard Hybrid III and the Hybrid III with the deformable face. These tests revealed that although the standard Hybrid III head produce a 40% higher peak acceleration, the 36 ms Head Injury Criterion (HIC) values were very similar. A potential limitation of this headform is that the data that the distributed loading performance was validated on was only preliminary data and may not be accurate for the severity range of interest. Melvin and Shee’s deformable Hybrid III face is still being used in more recent years[20][21] and is considered one of the most sophisticated ATD faces for zygoma, maxilla, and mandible impacts.
Cormier et al.'s FOCUS headform (2010)

In 2010, Cormier et al. conducted a study aimed at validating and assessing the biofidelity of the FOCUS (Facial and Ocular Countermeasure Safety) headform. The primary goal of this investigation was to gain insights into the response of human cadavers to blunt impacts and to compare this response with that of the FOCUS headform as previous studies were not able to due to the lack of available cadaveric data.
The FOCUS headform is equipped to measure the forces applied to both facial and orbital structures. It divides the face into eight distinct sensing regions, each of which overlaps with load cells[22]. These regions encompass the frontal bone, nasal bone, zygoma, maxilla, and mandible, as shown in Figure 10, constructed from rigid urethane plastic and firmly attached to load cells supported by an internal aluminum frame[22]. Additionally, the outer skin and nose insert are crafted from soft urethane material and the frangible eyes are mounted into the removable orbit of the headform with a ballistic gelatin solution[23].
To compare the stiffness of the nasal, maxilla, and frontal regions, tests involving the use of a rigid cylindrical aluminum impactor (3.2 kg) with a steel tip were conducted on both the FOCUS headform and 31 male cadavers, ranging in age from 43 to 94 years[22]. The results of the impact tests revealed that the maxilla and frontal regions of the FOCUS headform exhibited stiffness characteristics similar to the cadaver data. However, in the nasal region of the FOCUS headform, forces were found to be higher than anticipated from the cadaver data (~4000 N for the FOCUS headform as compared to ~1500 N for the cadaveric data), as there was an observed increase in stiffness as displacement increased[22]. As a result, this study suggests that the FOCUS nose should be made stiffer to enhance its biofidelity for that specific region[22]. Despite this limitation, the FOCUS headform does allow for a more comprehensive and detailed assessment of facial and ocular responses due to facial segmentation and its ability to predict eye injury risk.
Liu et al. THOR dummy (2021)
An iteration of the Hybrid III foundation, THOR's (Test device for Human Occupant Restraint) sensor technology shows improvements in accuracy and sensitivity, particularly in chest and head regions. While past research emphasized THOR's chest sensor sensitivity, rapid response, and shoulder structure, Liu et al. aim to provide a comprehensive comparison of head structures, calibration methods, and performance indexes between the Hybrid III and THOR crash test dummies[24]. THOR's head model is divided into forehead and facial sections, featuring five distinct facial sensors for heightened sensitivity whereas Hybrid III relies solely on a sensor at the center of mass and lacks facial sensors[24]. As well, the calibration methods are different for each dummy. Testing the Hybrid III involves suspending the head upside down for impact, while THOR uses seated forehead and facial tests. In the forehead test, the impactor strikes 30 mm above the eyebrow line, and in the facial test, it strikes at 68 mm below the bridge of the nose[24]. Furthermore, Table 1 shows higher peak detection power, peak head center of gravity result acceleration, and reference peak times of THOR as compared to Hybrid III. Ultimately, THOR's advanced design and calibration allow it to be more biofidelic in impact testing scenarios, potentially offering a replacement to the Hybrid III dummy.
| Hybrid III | THOR | |
|---|---|---|
| Peak Detection Power (N) | 5498 - 5660[24] | 9067 -11082[24] |
| Peak Head CG result acceleration (g) | 112.2 - 118.7[24] | 209 - 255[24] |
| Reference Peak Time (ms) | 2.0 - 2.4[24] | 4.42 - 5.4[24] |
Discussion
Different datasets give different parameters
One of the more difficult parts of developing ATD’s for detecting facial injuries is knowing the injury tolerances and forces at which injuries occur. The datasets used by the different sources throughout the study differed between each other, and are usually very small as cadaveric subjects are expensive to obtain and collect data from. This means the data used may differ from the general population.
Lacking of soft tissue damage evaluation
Some of the issues which can be seen throughout the development of dummy faces is the lack of depth in soft tissue damage and how injuries affect a patient psychologically. While facial injuries usually aren’t high on the AIS scale [14][16] Warner et al. (1986) mentioned as early as the 80’s that facial injuries are known to cause a long-term decrease in quality of life because of the social consequences arising from facial deformities and the change in self perception. While this had been known for a few years before Warner’s publishing, Newman and Gallup[14] mentions in 1984 that while the principal facial injuries are those to the soft tissue, the soft tissue of ATD’s at that time were not developed to account for lacerations occurring from impacts to relatively compliant surfaces but instead for impacts with sharp objects such as glass fragments meaning a large portion of soft tissue injuries were effectively overlooked at that time[14]. This being the case even though head/facial injuries were the most frequently occuring injury type in frontal crashes at the time showcases how cosmetic and soft tissue damages to the face were underrepresented during earlier ATD development[25]. Why this is the case could stem from one of the core issues with the AIS scale, as it only takes into account the risk of dying, a risk which facial injury usually isn't correlated with. [14][16]
The case for facial fractures at that time was different since fractures often produced injuries with higher scores on the AIS injury scale, but they were not fully developed. Newman and Gallup (1987) states that ATD’s used in frontal collision barrier car crash tests are able to predict injury locations quite accurately when compared to accident data [25]. Although this is limited to the rather specific case of frontal collision barrier impact tests where the dummy movement is “highly” predictable. In 1986 Nyqist et al. conducted a study to determine if ATD’s at that time were properly developed to assess injury risk of different types of facial injuries by comparing ATD tests to cadaver tests[3]. The key takeaway from their study was that the typical dummy head at the time was too stiff to provide proper acceleration data in facial impact environments although it is worth noting that this same year Warner et al. created a way to properly determine localized forces to ATD’s facial structures in a repeatable way[16].
The FOCUS headform showed a huge leap from earlier versions of ATDs with its division of different facial regions which gave it an increase in biofidelity, especially for fracture mechanisms, compared to earlier variants[22]. Still, laceration or abrasion injuries of the skin is barely mentioned leading to these types of damages being hard to predict from injury testing.
Variability in face geometry and injury tolerances
While some of the studies use cadaveric data from both male and female cadaveric specimens most of them don’t. One of the studies mentioning difference in strength for the female versus male bone structure is Newman and Gallups (1984), where they state that female’s facial bone structure have a significantly lower average strength[14], referencing a 1968 study. While this has been known for more than half a decade, the 2010 study done on the FOCUS headform only used data from male cadaveric subjects[22]. Why female anatomy and biomechanics are underrepresented in research stems from the roots of how society today is built. In short and very simply described, since an ATD isn't able to resemble all groups of people, and the people developing the ATD's have predominantly been male, the ATD's themselves have historically been developed to resemble men. This causes females to be put at a much higher risk of injuries in a wide variety of situations including car crashes, where they face a 47% higher risk of serious injuries compared to men[26].
There also seems to be a lack of understanding and research in how different facial geometries impact injury mechanics. Nyquist mentions that different facial geometries, especially ones of the nasal bone, seem to give a large variety in how easily nasal fractures occur[3]. This was also mentioned in Cormier et al’s. study, as tests showed a great variation of force-displacement response which also meant the nasal bone response of FOCUS, while staying within the human corridor, was still far from the outer values of the force-displacement corridor[22]. Something which might be able to fill this gap is the advancing of FEM-models such as the one developed by Mao et al., whose facial geometries can be varied to take these issues into account[27]. Although these are not flawless, as Mao et al. mentions there is still improvement needed for region specific bone failure criteria aswell as other material deviations. The model also provides a good way of calculating brain accelerations, giving a better prediction of brain injury[27].
Limitations and Future Research
Although a significant effort has been made towards improving the accuracy of replicating human facial injuries in car crashes using ATDs, the researchers suggest that there are still limitations to accurately detect human facial injuries.
Biofidelity Improvements of Hybrid III
Researchers were able to improve the biofidelity of Hybrid III headform by conducting cadaver head impact studies and facial bone studies[14]. This was done by modifying the skull stiffness, adding a frangible faceform, and including a more flexible mandible. The main limitation is that they did not simulate the rotational forces during the car crash tests. During an actual collision, the head often undergoes rotational movements, which may lead to various injury mechanisms. Therefore, neglecting the rotational can significantly impact the understanding of facial injury patterns during an actual accident.
GM Hybrid III Deformable Face
Another group of researchers focused on analyzing the biomechanical behavior of the facial tissues and bones under localized and distributed loads in the context of car crashes[13]. Ultimately, they integrated the developed GM Hybrid III Deformable face into the existing Hybrid lll. While they were successfully able to measure the frontal impact response for localized and distributed facial loads, their simulations were restricted to the mentioned type of loads and a specific crash scenario (wheel hub load), limiting the understanding of the impact on facial injuries in other crash scenarios. Additionally, the deformable face head was developed for the Hybrid III mid-size male, which does not account for female passengers or any passenger with a smaller or bigger head size. Similar to the Hybrid III simulation, the rotational movements were neglected. In this case, possible facial injuries due to rotational movements are being neglected, which limits the information obtained from this simulation.
To address these limitations, future research is needed to enhance the understanding of human facial injuries in the context of car crashes to ultimately design safer vehicle features and set safety regulations, preventing such injuries.
To date, it has been obtained that facial bone fractures are prevalent in motor vehicle accidents[5]. Therefore, it is essential to use data associated with force tolerance of different facial bones while designing more biofidelic ATDs to replicate human facial responses under accident more accurately.
As mentioned previously, neglecting rotational forces limits the understanding of facial injury patterns[13][14]. Therefore, future research should focus on enhancing the biofidelity of the ATDs and being able to simulate rotational forces that may occur during a real-world car accident to replicate more accurate real-world car accidents. Expanding the simulation scenarios (such as rollover and collision from different angles) can contribute to comprehensively understanding facial injuries in diverse situations.
It is also important to highlight the Equity, Diversity, and Inclusion (EDI) consideration in the context of Facial Load Sensors for ATDs. Researchers have primarily used male ATDs [13][14][16]. The physiological differences in females and individuals with different head sizes should be considered in future research to ensure that the car crash tests are applicable to a broad range of individuals, promoting safety and inclusivity in automotive designs.
References
- ↑ J. K. Foster, J. O. Kortge, and M. J. Wolanin, “Hybrid III-A Biomechanically-Based Crash Test Dummy,” SAE International, Warrendale, PA, SAE Technical Paper 770938, Feb. 1977. doi: 10.4271/770938.
- ↑ J. C. McCarty et al., “Long-Term Functional Outcomes of Trauma Patients With Facial Injuries,” J. Craniofac. Surg., vol. 32, no. 8, p. 2584, Dec. 2021, doi: 10.1097/SCS.0000000000007818.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 G. W. Nyquist, J. M. Cavanaugh, S. J. Goldberg, and A. I. King, “Facial Impact Tolerance and Response,” SAE Trans., vol. 95, pp. 850–871, 1986.
- ↑ 4.0 4.1 M. Yu and S.-M. Wang, “Anatomy, Head and Neck, Zygomatic,” in StatPearls, Treasure Island (FL): StatPearls Publishing, 2023. Accessed: Nov. 06, 2023. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK544257/
- ↑ 5.0 5.1 5.2 5.3 5.4 “Analysis of Traffic Accident-Related Facial Trauma : Journal of Craniofacial Surgery.” Accessed: Nov. 06, 2023. [Online]. Available: https://journals.lww.com/jcraniofacialsurgery/abstract/2016/10000/analysis_of_traffic_accident_related_facial_trauma.17.aspx
- ↑ S. Menon et al., “Maxillofacial Fracture Patterns in Road Traffic Accidents,” Ann. Maxillofac. Surg., vol. 9, no. 2, pp. 345–348, 2019, doi: 10.4103/ams.ams_136_19.
- ↑ E. M. Peltola, M. P. Koivikko, and S. K. Koskinen, “The spectrum of facial fractures in motor vehicle accidents: an MDCT study of 374 patients,” Emerg. Radiol., vol. 21, no. 2, pp. 165–171, Apr. 2014, doi: 10.1007/s10140-013-1173-1.
- ↑ J. T. Hefner and K. C. Linde, “Chapter 9 - Nasal Bone Contour,” in Atlas of Human Cranial Macromorphoscopic Traits, J. T. Hefner and K. C. Linde, Eds., Academic Press, 2018, pp. 105–124. doi: 10.1016/B978-0-12-814385-8.00009-4.
- ↑ J. Cormier et al., “The tolerance of the nasal bone to blunt impact,” Ann. Adv. Automot. Med. Assoc. Adv. Automot. Med. Annu. Sci. Conf., vol. 54, pp. 3–14, 2010.
- ↑ V. R. Hodgson, “Tolerance of the facial bones to impact,” Am. J. Anat., vol. 120, no. 1, pp. 113–122, 1967, doi: 10.1002/aja.1001200109.
- ↑ J. J. Dutton, “CHAPTER 3 - Anatomy of the Orbit,” in Radiology of the Orbit and Visual Pathways, J. J. Dutton, Ed., London: W.B. Saunders, 2010, pp. 31–39. doi: 10.1016/B978-1-4377-1151-6.00003-3.
- ↑ 12.0 12.1 12.2 12.3 12.4 J. W. Melvin, P. M. Fuller, R. P. Daniel, and G. M. Pavliscak, “Human Head and Knee Tolerance to Localized Impacts,” SAE Trans., vol. 78, pp. 1772–1782, 1969.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 J. W. Melvin, W. C. Little, J. Smrcka, Y. Zhu, and M. J. Salloum, “A Biomechanical Face for the Hybrid III Dummy,” SAE Trans., vol. 104, pp. 3016–3028, 1995.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 J. A. Newman and B. M. Gallup, “Biofidelity Improvements to the Hybrid III Headform,” SAE International, Warrendale, PA, SAE Technical Paper 841659, Oct. 1984. doi: 10.4271/841659.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 C. Tarrière, Y. C. Leung, A. Fayon, C. Got, A. Patel, and P. Banzet, “Field Facial Injuries and Study of Their Simulation with Dummy,” SAE Trans., vol. 90, pp. 3167–3180, 1981.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 C. Y. Warner, M. G. Wille, S. R. Brown, S. Nilsson, H. Mellander, and M. Koch, “A Load Sensing Face Form for Automotive Collision Crash Dummy Instrumentation,” SAE Trans., vol. 95, pp. 1009–1020, 1986.
- ↑ D. C. Schneider and A. M. Nahum, “Impact Studies of Facial Bones and Skull,” SAE International, Warrendale, PA, SAE Technical Paper 720965, Feb. 1972. doi: 10.4271/720965.
- ↑ K. Ono, A. Kikuchi, M. Nakamura, H. Kobayashi, and N. Nakamura, “Human Head Tolerance to Sagittal Impact Reliable Estimation Deduced from Experimental Head Injury Using Subhuman Primates and Human Cadaver Skulls,” SAE International, Warrendale, PA, SAE Technical Paper 801303, Sep. 1980. doi: 10.4271/801303.
- ↑ 19.0 19.1 D. “L” Allsop, C. Y. Warner, M. G. Wille, D. C. Schneider, and A. M. Nahum, “Facial Impact Response — A Comparison of the Hybrid III Dummy and Human Cadaver,” SAE Trans., vol. 97, pp. 1224–1240, 1988.
- ↑ D. C. Viano, C. Bir, T. Walilko, and D. Sherman, “Ballistic impact to the forehead, Zygoma, and mandible: Comparison of human and frangible dummy face biomechanics,” The Journal of Trauma: Injury, Infection, and Critical Care, vol. 56, no. 6, pp. 1305–1311, 2004. doi:10.1097/01.ta.0000064209.21216.4e
- ↑ T. J. Walilko, D. C. Viano, and C. A. Bir, “Biomechanics of the head for Olympic boxer punches to the face,” British Journal of Sports Medicine, vol. 39, no. 10, pp. 710–719, 2005. doi:10.1136/bjsm.2004.014126
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 22.7 J. Cormier et al., “Biomechanical Response of the Human Face and Corresponding Biofidelity of the FOCUS Headform,” SAE Int. J. Passeng. Cars - Mech. Syst., vol. 3, no. 1, Art. no. 2010-01–1317, Apr. 2010, doi: 10.4271/2010-01-1317.
- ↑ “Design of an Advanced Headform for the Prediction of Eye and Facial Injuries.” Accessed: Nov. 06, 2023. [Online]. Available: https://apps.dtic.mil/sti/citations/ADA481591
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 24.8 Z. Liu, W. Liu, W. Ma and B. Duan, "Research on the difference of head calibration between the THOR 50M dummy and HYBRID III 50th dummy," 2021 International Conference of Social Computing and Digital Economy (ICSCDE), Chongqing, China, 2021, pp. 280-283, doi: 10.1109/ICSCDE54196.2021.00071.
- ↑ 25.0 25.1 B. M. Gallup and J. A. Newman, “The Assessment of Facial Injury to Fully Restrained Drivers through Full-Scale Car Crash Testing,” J. Trauma Acute Care Surg., vol. 27, no. 7, p. 711, Jul. 1987.
- ↑ Perez, Caroline (2023-02-23). "The deadly truth about a world built for men – from stab vests to car crashes". The Guardian. Retrieved 2023-12-02.
- ↑ 27.0 27.1 H. Mao et al., “Development of a Finite Element Human Head Model Partially Validated With Thirty Five Experimental Cases,” J. Biomech. Eng., vol. 135, no. 111002, Sep. 2013, doi: 10.1115/1.4025101.