Course:PostgradFamilyPractice/ExamPrep/99 Priority Topics/Pneumonia
Pneumonia - Key Features
Community-Acquired Pneumonia (CAP) – pneumonia contracted in the community, specifically not in a hospital or a long-term care facility.
Healthcare-Associated Pneumonia (HAP) (hospital-acquired pneumonia) – pneumonia contracted by a patient meeting any of the following criteria:
- • admitted to a hospital for ≥2 days in the preceding 3 months
- • living in a long-term care facility
- • treated with IV antibiotics, dialysis, chemotherapy or wound care in the preceding month
- • has a family member infected with a multidrug-resistant pathogen
1. In a patient who presents without the classic respiratory signs and symptoms (e.g. deterioration, delirium, abdominal pain), include pneumonia in the differential diagnosis.
In otherwise healthy adults, the classic symptoms of pneumonia include new onset cough (productive or non-productive, pathogen-dependent), fever/chills/rigours, dyspnea, and pleuritic chest pain. The classic physical exam findings (tachypnea, respiratory crackles, bronchial breath sounds, dullness to percussion, and increased vocal fremitus) are definitely suggestive of a focal pneumonia but are neither sensitive nor specific. While the absence of fever or crackles/consolidation findings on physical exam makes a significant lobar pneumonia unlikely, their absence does not rule out bronchopneumonia or small focal pneumonias. No combination of signs and symptoms has been found to rule in or out pneumonia with any certainty.
Non-classic symptoms of pneumonia can include new onset mental confusion (especially in the elderly), GI upset (nausea, vomiting and diarrhea), headache, fatigue, and myalgias. The elderly are more likely to present with non-classic symptoms, and often do not mount a fever or elevated WBC count in response to infection. In addition, it is not uncommon for children with pneumonia to present with predominantly GI symptoms.
2. In a patient with signs and symptoms of pneumonia, do not rule out the diagnosis of a normal chest X-ray film (e.g., consider dehydration, neutropenia, human immunodeficiency virus [HIV] infection).
Chest X-ray remains the gold standard for diagnosing pneumonia in both adults and children. There is level II evidence recommending that all adult patients in whom pneumonia is suspected should have a chest X-ray to confirm the diagnosis. However, it is often argues that only children in respiratory distress necessitate a confirmatory chest X-ray.
False negative chest X-rays can occur, especially in patients with dehydration, severe neutropenia, PCP pneumonia, HIV, or in the first 24 hours of infection, false negative chest X-rays are possible.
3. In a patient with a diagnosis of pneumonia, assess the risks for unusual pathogens (e.g., a history of tuberculosis, exposure to birds, travel, HIV infection, aspiration).
The most common pathogen for community-acquired pneumonia in adults is Streptococcus pneumonia (>50% of bacterial pneumonia cases). Haemophilus influenza, Mycoplasma and Chlamydia pneumoniaes are not uncommon causes of CAP. Note, however, that the specific bacterial pathogen is identified in <50% of cases.
Healthcare-associated pneumonia (or hospital-acquired pneumonia) may be caused by multiple varying pathogens and polymicrobial infections are not uncommon. The most common HAP pathogens are Staph aureus, Strep pneumonia, Klebsiella, Acinetobacter, and Pseudomonas. In addition, these patients are at increased risk of multidrug resistant infection, most commonly MRSA and drug-resistant Strep pneumoniae (DRSP).
In children, age is the best predictor of bacterial pneumonia pathogen though as with adults, the responsible pathogen is not identified in 40 – 60% of cases. Viruses are the most common cause of pneumonia in children under 2 years of age, while in school-aged children, pneumonia is mostly commonly due to Strep and Mycoplasma pneumoniaes.
Elderly patients are at increased risk of having tuberculosis (especially those living in long-term care facilities), multi-drug resistant and gram negative organisms (especially elderly patients with decreased functional status and/or with multiple comorbid conditions). Patients with decreased level of consciousness for any reason are at risk of aspirating and thereby developing aspiration pneumonia (usually anaerobic pathogens) and/or chemical pneumonitis.
It is important to inquire about the patient’s travel history (e.g. possible risk of tuberculosis, fungal infection, etc) and living/working environment (e.g. risk of Legionella pneumophila in patients exposed to contaminated air conditioning, hot tubs, humidifiers, etc. or risk of Coxiella burneii in patients exposed to infected farm animals). Past medical history is also very important to consider as specific co-morbidities make patients susceptible to more uncommon pneumonia pathogens (e.g. patients with HIV are at increased risk of PCP pneumonia, COPD increases the risk for Haemophilus influenzae and Moraxella catarrhalis, and bronchiectasis increases the risk for Pseudomonas aeruginosa infection.
Finally, in addition to HAP, numerous factors increase a patient’s risk of infection with multi-drug resistant bacteria. Risk factors for MRSA infection include
- • homelessness
- • incarceration
- • IV drug abuse
- • First Nations persons living on reserves
- • healthcare workers
- • recent hospitalization (even admissions that don’t meet criteria for HAP)
Risk factors for DRSP include
- • age >65 years
- • antibiotic use within the preceding 3 months
- • exposure to children attending daycare facilities
- • co-morbid conditions including (but not limited to) pulmonary, cardiac, renal or liver disease; alcoholism; diabetes; malignancy; immunosupression; etc.
4. In patients with pre-existing medical problems (e.g., asthma, diabetes, congestive heart failure) and a new diagnosis of pneumonia:
a) Treat both problems concurrently (e.g., with prednisone plus antibiotics).
It is important to consider the effect the pre-existing condition may have on the pneumonia and the effect the pneumonia may have on the pre-existing condition. For example, asthma and COPD increase the risk of developing pneumonia and may prolong the course or worsen the severity of pneumonia. On the other hand, infection and the resulting cough both act to inflame the airways, thereby worsening the patient’s asthma/COPD symptoms. Thus, successful treatment of the pneumonia (with antibiotics) necessitates effective treatment of the asthma flare (usually with steroids).
b) Adjust the treatment plan for pneumonia, taking into account the concomitant medical problems (e.g., be aware of any drug interactions, such as that between warfarin [Coumadin] and antibiotics).
Antibiotics used in the treatment of pneumonia (macrolides, penicillins, and fluoroquinolones) can enhance the anticoagulant effects of warfarin. It is recommended that patients on warfarin undergo increased INR/PT monitoring when starting on or changing the dose of these antibiotics.
Macrolides and fluoroquinolones must not be given to patients on QTc-prolonging medications as there is moderate to severe increased risk of QTc-prolongation and/or serious arrhythmias in these patients. Both antibiotic families also decrease the absorption of typhoid vaccine (thereby diminishing its therapeutic effect) and thus concomitant use should be avoided.
Amoxicillin and several common medications interact to increase or decrease serum concentrations of one or both medications, increasing the risk of either toxic effects and/or diminishing the therapeutic effectiveness of these medications. Examples of medications that can diminish the therapeutic effectiveness of amoxicillin include fusidic acid and tetracycline derivatives while Probenecid increases amoxicillin serum concentrations. Amoxicillin is known to increase serum concentrations of methotrexate and vitamin K antagonists (warfarin) while it decreases the serum concentrations of estrogen contraceptives (minor), mycophenolate, and typhoid vaccines.
(*Please note, the above lists are in no way exhaustive.*)
5. Identify patients, through history-taking, physical examination, and testing, who are at high risk for a complicated course of pneumonia and would benefit from hospitalization, even though clinically they may appear stable.
There is no substitute for physician impression and judgement, and a decision whether or not to hospitalize a patient must take into account subjective factors such as a patient’s living conditions, availability of support, compliance with medications, and ability to return for follow-up care. That being said, several severity-of-illness tools are available to assist physicians in deciding on whether to hospitalize a patient or treating them as an outpatient. Many of these tools/calculators require several lab test results which are often not immediately available in the GP’s office [ex. the Pneumonia Severity Index (available at http://pda.ahrq.gov/clinic/psi/psicalc.asp) and the CURB-65 tool). A reliable severity tool that does not require immediate lab results is the modified CURB-65 tool. The Confusion, Respiratory rate, Blood pressure, age >65 years (CRB-65) tool has been validated in the primary care setting. The following table (from the May 2009 McMaster Module, “Pneumonia in Adults”, © The Foundation of Medical Practice Education, www.fmpe.org) explains the tool.
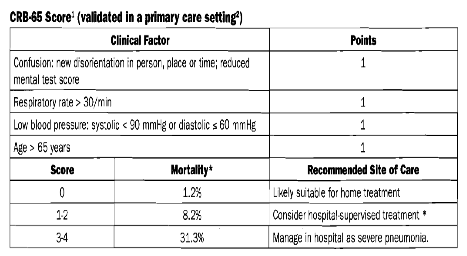
Thus, hospitalization should be considered for any patient with a CRB-65 score of ≥1. Hospitalization is indicated in patients with a score ≥3, are unable to take oral medications and/or are hypoxic (Sp02 <90%).
6. In the patient with pneumonia and early signs of respiratory distress, assess, and reassess periodically, the need for respiratory support (bilevel positive airway pressure, continuous positive airway pressure, intubation) (i.e., look for the need before decompensation occurs).
There are several major and minor criteria that help to identify the patient who is at increased risk of requiring respiratory support and/or ICU admission. These criteria are as follows:
Major Criteria
- • invasive mechanical ventilation
- • septic shock requiring vasopressors
Minor Criteria
- • respiratory rate ≥30
- • temperature <36⁰C
- • hypotension requiring aggressive fluids or vasopressors
- • new-onset confusion or disorientation
- • multilobar infiltrates
- • PaO2/FiO2 ≤250
- • urea >7 mmol/L
- • WBC <4
- • platelets <100
Patients with 1 major or ≥3 minor criteria likely require ICU admission. Respiratory support (including BiPAP, CPAP, and intubation) should be considered whenever a patient is in respiratory distressed or hypoxic (Sp02 <90) and respiratory support should be initiated (wherever possible) before decompensation occurs.
7. For a patient with a confirmed diagnosis of pneumonia, make rational antibiotic choices (e.g., outpatient + healthy = first-line antibiotics; avoid the routine use of “big guns”).
A. As Strep pneumoniae is the single most common cause of pneumonia in adults, approach to treatment is determined by a patient’s risk for -resistant Strep pneumoniae (DRSP).
Adults with Community-Acquired Pneumonia (Outpatient Treatment):
- • For otherwise healthy adults who are at low risk of multi-drug resistant infection should be treated with a macrolide (clarithromycin, azithromycin, or erythromycin). Patients who cannot tolerate a macrolide should be treated with doxycycline or a respiratory fluoroquinolone (moxifloxacin, levofloxacin, or gemifloxacin).
- • Adults who are at increased risk for drug-resistant DRSP should be treated with either a respiratory fluoroquinolone or combined therapy with a ß-lactam (amoxicillin or amoxicillin/clavulanate) AND a macrolide.
- • Patients at high risk for MRSA should have vancomycin or linezolid in addition to the above antibiotic regime.
Adults with Community or Healthcare-Acquired Pneumonia (Inpatient Treatment):
- • Hospitalized patients at low risk for DRSP or MRSA should receive monotherapy or either a respiratory fluoroquinolone or the combination of a ß-lactam (in this case ampicillin, ceftriaxone or cefotaxime) AND a macrolide.
- • Hospitalized patients who are at increased risk for DRSP should receive combination therapy of
- 1) a ß-lactam (in this case piperacillin-tazobactam) or an antipseudomonal cephalosporin (cefepime or ceftazidime) or an antipseudomonal carbapenem (imipenem or meropenem) AND
- 2) an antipseudomonal fluoroquinolone (ciprofloxacin or levofloxacin) or both azithromycin and an aminoglycoside.
- • Patients at high risk for MRSA, in addition to the above regime, should receive
- 3) vancomycin or linezolid
Adults with Inpatient ICU-Treated Pneumonia:
- • Patients at low risk for DRSP should receive combination therapy with
- 1) a ß-lactam (in this case ceftriaxone or cefotaxime) AND
- 2) azithromycin or a respiratory fluoroquinolone
- • Patients who are at high risk for DRSP should receive combination therapy with
- 1) a ß-lactam (in this case piperacillin-tazobactam) or an antipseudomonal cephalosporin or an antipseudomonal carbepenem AND
- 2) an antipseudomonal fluoroquinolone or both azithromycin and an aminoglycoside
- • Patients at high risk for MRSA, in addition to the above regime, should receive
- 3) vancomycin or linezolid
- • Penicillin-allergic patients who are at low risk for DRSP should be treated with a respiratory fluoroquinolone AND an aminoglycoside (as well as vancomycin or linezolid if they are at increased risk for MRSA)
B. Since the most common pathogens in pediatric pneumonia change with a child’s age, the approach to treatment also changes with the child’s age.
Children with Community-Acquired Pneumonia (Outpatient Treated):
- • 3 months – 5 years:
- o amoxicillin or
- o a macrolide (if ß-lactam allergic)
- • >5 years:
- o a macrolide or
- o doxycycline (if >8 years)
Children with Community or Hospital-Acquired Pneumonia (Inpatient Treated):
- • 1 – 3 months (pneumonitis syndrome)
- o a macrolide
- • 1 – 3 months (bacterial pneumonia – consider referral)
- o cefuroxime
- • 3 months to 5 years
- o cefuroxime
- • >5 years
- o cefuroxime and
- o a macrolide (azithromycin or erythromycin only)
Critically Ill Children with Pneumonia: (*consider referral*)
- • 1 – 3 months (pneumonitis syndrome)
- o a macrolide (azithromycin or erythromycin only)
- • 1 – 3 months (bacterial pneumonia)
- o cefuroxime or
- o cefotaxime and cloxacillin
- • 3 months – 5 years
- o cefuroxime and erythromycin or
- o cefotaxime and cloxacillin
- • >5 years
- o azithromycin or
- o cefuroxime and erythromycin
8. In a patient who is receiving treatment for pneumonia and is not responding:
a) Revise the diagnosis (e.g., identify other or contributing causes, such as cancer, chronic obstructive pulmonary disease, or bronchospasm), consider atypical pathogens (e.g., Pneumocystis carinii,TB, and diagnose complications (e.g., empyema, pneumothorax).
Most patients are expected to improve clinically within the first 3 days of starting appropriate antibiotic therapy. If a patient deteriorates or shows no improvement within 72 hours of treatment initiation, it is important to consider the following possibilities:
- • incomplete antibiotic coverage
- o atypical pathogen (TB, fungal infection, etc.)
- • antibiotic-resistant organism
- • parapneumonic effusion
- • empyema
- • pneumothorax
- • undiagnosed underlying condition (e.g. in children, cystic fibrosis; in adults, malignancy)
- • incorrect diagnosis
- o pulmonary embolus
- o congestive heart failure
- o foreign body aspiration
- o chest wall pathology, etc.
b) Modify the therapy appropriately (e.g., change antibiotics).
Consider expanding the spectrum of antibiotic coverage, repeating the chest X-ray, investigating further (e.g. blood and/or sputum cultures for atypical organisms), etc.
9. Identify patients (e.g., the elderly, nursing home residents, debilitated patients) who would benefit from immunization or other treatments (e.g., flu vaccine, Pneumovax, ribavarine) to reduce the incidence of pneumonia.
PNEUMOCOCCAL VACCINE:
The Public Health Agency of Canada currently recommends the pneumococcal vaccine in the following situations:
Children
- • all children age ≤23 months
- • children age ≥24 months who have not previously received the vaccine and who have any of the following risk factors for invasive pneumococcal disease:
- o functional or anatomic asplenia
- o sickle cell disease
- o HIV
- o primary immunodeficiency
- o malignancy
- o immunosuppressive therapy
- o solid organ transplant
- o nephritic syndrome
- o chronic cardiac, renal, hepatic, or pulmonary disease
- o bronchopulmonary dysplasia
- o diabetes
- o CSF leak
- o First Nations children
- o children attending daycare facilities
Adults
- • age ≥65 years
- • current smokers
- • cirrhosis
- • alcoholism
- • unknown immunization history
- • any of the risk factors for IPD listed above (for children ≥5 years)
INFLUENZA VACCINE:
As influenza complications (including secondary bacterial pneumonia) are a significant cause of morbidity and mortality, the Public Health Agency of Canada currently recommends a yearly influenza vaccine to people who meet any of the following criteria:
- • adults age ≥65 years
- • healthy children age 6 – 23 months
- • residents of long-term care facilities
- • health care workers
- • household contacts of
- o children <6 months of age
- o people at increased risk of influenza complications or IPD
- • people with chronic medical conditions requiring regular medical care
All patients should be counselled on the importance of hand washing to prevent the spread of viral infections that can predispose to pneumonia. As smoking is the strongest independent risk factor for IPD, counselling and support for smoking cessation and avoidance of second-hand smoke are critical for pneumonia prevention.
10. In patients with a diagnosis of pneumonia, ensure appropriate follow-up care (e.g., patient education, repeat chest X-ray examination, instructions to return if the condition worsens).
Patients must be counselled on signs and symptoms of illness progression and when to return to clinic and/or go proceed to the local emergency department. Patients should be seen in follow-up in any of the following is true:
- • illness progression despite antibiotic therapy
- • no improvement within 72 hours of antibiotic initiation
- • patients nearing the end of their antibiotic course who have not achieved at least two of the following sings of clinical stability:
- o temperature ≤37.8oC for at least 48 – 72 hours
- o heart rate <100
- o respiratory rate ≤24
- o systolic blood pressure >90
- o arterial oxygen saturation ≥90% or PO2 ≥60mmHg on room air
- o ability to tolerate oral intake
- o return to baseline mental status
11. In patients with a confirmed diagnosis of pneumonia, arrange contact tracing when appropriate (e.g., in those with TB, nursing home residents, those with legionnaires’ disease).
All confirmed cases of the following infections are nationally-reportable:
- • Tuberculosis
- • Legionella
- • invasive Group A Strep (Strep pyogenes)
- • laboratory-confirmed Influenza
- • Hantavirus Pulmonary Syndrome
- • Severe Acute Respiratory Syndrome (SARS)
In addition, contact tracing for either close monitoring and/or prophylactic treatment should be done for all patients with pneumonia confirmed to be caused by any of the above pathogens. Contacts include anyone who has been exposed to the patient in the time period from one week prior to the patient’s symptom onset to 24 hours after the patient has started appropriate antimicrobial therapy and who has any of the following relationships with the patient:
- • co-residents of long-term care facilities
- • co-attendants of child care centres,
- • IV drug users who have shared needles with the patient
- • sexual partners or share the same bed with the patient
- • household contacts who have spent an average of >4 hours/day with the patient
- • anyone who has had direct mucous membrane contact with the oral or nasal secretions or direct contact with an open skin lesion of the patient.
Study Guide
Resources
Pneumonia Severity Index http://pda.ahrq.gov/clinic/psi/psicalc.asp
The Foundation of Medical Practice Education Pneumonia in Adults www.fmpe.org/index.asp
CRB-65 Severity score for community-acquired pneumonia www.aafp.org/fpm/2006/0400/fpm20060400p41-rt2.pdf