Course:PostgradFamilyPractice/ExamPrep/99 Priority Topics/LOC
Loss of Consciousness - Key Features
1. In an unconscious patient, assess ABC’s and resuscitate as needed.
2 As part of the assessment of a patient who has lost consciousness, obtain focused history from the patient or witnesses that would include duration, trauma, preexisting conditions, drugs, toxins, medications and seizure activity.
3 Examine unconscious patients for localizing and diagnostic signs (e.g., ketone smell, liver flap, focal neurologic signs).
4 In patients with a loss of consciousness and a history of head trauma, rule out intracranial bleeding.
5 In patients with a loss of consciousness who are anticoagulated, rule out intracranial bleeding.
6 Assess and treat unconscious patients urgently for reversible conditions (e.g., shock, hypoxia, hypoglycemia, hyperglycemia, and narcotic overdose).
7 When following up patients who have lost consciousness, assess and advise regarding return to work, sporting, driving and recreational activities to minimize the possibility of injury to self or others in the event of a recurrence.
8 In patients who have had a loss of consciousness without a clear diagnosis, pursue investigations (e.g., rule out transient arythmia, seizure).
9 When following up patients who have lost consciousness and where there is potential for recurrent episodes, discuss specific preventive and protective measures (e.g., position changes with orthostatic pressure changes).
10 In patients with loss of consciousness following head trauma, treat and follow up according to current concussion guidelines.
11 Advise authorities about appropriate patients with loss of consciousness (e.g., regarding driving status).
1. Initial Assessment:
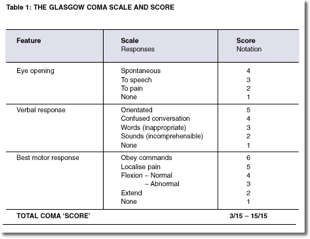
- Airway - place prone, assess for trauma, breath sounds, place O2 and intubate as needed (GCS < 8)
- Breathing - equal breath sounds, SpO2
- Circulation - general appearance, warmth, pulses, get ECG leads in place, assess for arrythmias/shockable rhythm, get 2 X large bore IV access
Coma Cocktail (Empiric mgmt): IV Bolus: D50W 50 cc, thiamine 100 mg, narcan 0.2-0.4 mg
2. Differential dx
Most cases of stupor and coma presenting to an emergency department are due to trauma, cerebrovascular disease, intoxications, and metabolic derangements (UTD)
Structural: trauma, bleed, clot, fat emboli, vasculitis, MS (very long list of other differential), Cardiac (arrythmia) can be included in this category
ASK: hx of trauma, onset of symptoms (ie, abrupt R/O SA hemorrhage), preceding symptoms (ie, visual change suggests ischemia in posterior circulation)
Non-structural:
- Drugs: Sedatives, Barbiturates, Other hypnotics, Tranquilizers, Bromides, Alcohol, Opiates, Paraldehyde, Salicylate, Psychotropics, Anticholinergics, Amphetamines, Lithium, Phencylidine Monoamine oxidase inhibitors
- Toxins: Lead, Thallium, Mushrooms, Cyanide, Methanol, Ethylene glycol, Carbon monoxide
- ASK: Medication use, compliance, substance history, access to substances, ability to use meds appropriately,
- Infection: Bacterial meningitis Viral encephalitis Postinfectious encephalomyelitis Syphilis Sepsis Typhoid fever Malaria
- ASK: prodromal illness, fever, neck stiffness, travel, sick contacts, headache
- Metabolic: Hypoxia Hypercapnia Hypernatremia* Hypoglycemia* Hypergylcemic nonketotic coma Diabetic ketoacidosis Lactic acidosis Hypercalcemia Hypocalcemia Hypermagnesemia Hyperthermia Hypothermia Reye's encephalopathy Aminoacidemia Wernicke's encephalopathy Porphyria Hepatic encephalopathy* Uremia Dialysis encephalopathy Addisonian crisis Hypothyroidism
- Psychiatric: Catatonia, pseudo-seizure
- Other: seizure with post-ictal period, non-convulsive status epilepticus, hypotension
**Consider also for ddx: Neuro vs Non-neuro**
3. Physical Exam
Vitals, pupil size & reactivity (usually spared in metabolic coma) EOM, fundi, corneal reflexes, motor reflexes, respiratory patterns. Waxing and waning LOC typical of metabolic coma
Infection: fever, meningismus, septic signs
Herniation: hypertension with bradycardia
Resp: hyperventilation often due to metabolic acidosis (methanol, salicylates, DKA, uremia, lactic) or resp alkalosis (sepsis, hepatic failure, heart failure)
Cheyne-Stokes respirations (a pattern of periodic waxing then waning hyperpnea, followed by brief apnea) may occur with either impaired cardiac output or bicerebral dysfunction, and also in elderly patients during sleep.
Toxidromes:
TCA overdose: hypotension, tachycardia, wide QRS, anticholinergic SE’s.
benzos overdose: *unlikely to alter VS unless co-ingestion* usually CNS changes with N vitals
anticholinergic: red, hot, dry, CNS disturbed, vis disturbance
amphetamine: *more likely agitated than obtunded* tachycardia, hypertension, agitation
opioid: decreased resp rate, pinpoint pupils
4. Investigations
BW: CBC, lytes, BS, Bun, Creat, lactate, LFTs, ABGs, cultures, Ca, Albumin, INR, PTT, capillary bld sugar, drug screen (based on clinical setting)
ECG, CT head (see below), consider LP based on findings
*For trauma/post concussion see Canadian CT Head Rules *
5. Treatment
Sepsis: Early fluids, empiric antibiotics, locate source
Overdose treatments:
- hypoglycemia: 1 amp D50W, may need IV D5W infusion following
- hyperglycemia: fluids followed by insulin (see DKA protocols)
- benzos: flumazenil
- acetaminophen: NAC (use normogram to assess need)
- TCA: sodium bicarb infusion (for widened QRS), vasopressors if necessary following
- Opiate: naloxone (Narcan) 0.2-0.4 mg to start- titrate with clinical benefit- watch for withdrawal
- beta blocker or Ca channel blocker: calcium and glucagon
CNS infection: get LP first if possible, however if IV empiric indicated: IV ceftriaxone
Head Trauma: elevate head of bed (20-30 degrees, helps increase venous outflow and decrease ICP, hyperventilate, prevent hypotension (fluids), blood type & screen
Consider C-spine injury and C-spine precautions!
6. Follow up
Head Trauma: See www.thinkfirst.ca
Concussion assessment/mgmt (after brief LOC):
Signs of a structural brain injury could include: increasing headaches, decreasing LOC, increasing tiredness and confusion, any lateralizing weakness, seizure temporally remote from the injury, persistent vomiting.
Remember to examine neck, jaw, facial structures- blow to these areas can cause concussion. Full neurologic assessment, tests of memory, orientation, concentration
Return to work/sport: Being “asymptomatic” refers to physical, cognitive, and emotional manifestations of concussion. Any time symptoms reoccur, patients should take a step back from activity
Seizure: Driving guidelines: http://www.cmaj.ca/content/168/4/441/T4.expansion.html
Study Guide
Resources
Uptodate
Canadian CT Head Rule www.ohri.ca/emerg/cdr/cthead.html
Head trauma follow up www.thinkfirst.ca/index.aspx
Driving guidelines in seizures www.cmaj.ca/content/168/4/441/T4.expansion.html