Course:PostgradFamilyPractice/ExamPrep/99 Priority Topics/IHD
Ischemic Heart Disease - Key Features
1. Given a specific clinical scenario in the office or emergency setting, diagnose presentations of ischemic heart disease (IHD) that are:
- classic
- atypical (e.g., in women, those with diabetes, the young, those at no risk).
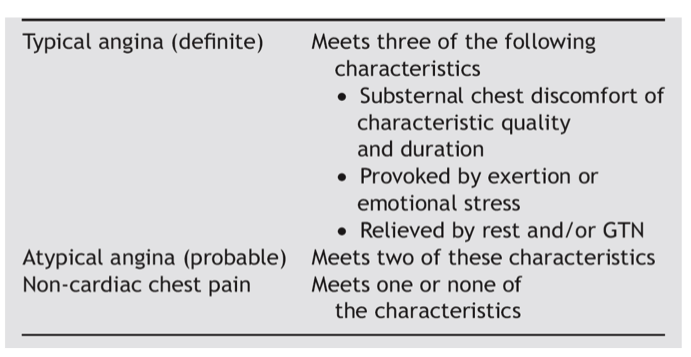
IHD refers to a variable degrees of myocardial ischemia from an imbalance between oxygen supply and demand resulting from narrowing of vessels. In stable angina, predictably exertion and emotional changes where demand increases or eating where supply decreases lead to presentation of angina symptoms. Once the increased demand is mitigated by stopping activity or an increase in supply is provided by nitrates, symptoms resolve. Classically patients will complain of retrosternal chest pain, discomfort, tightness, pressure, squeezing, or fullness which may radiate into the arms, neck, jaw, shoulder or back and associated with nausea, fatigue, SOB, sweating, or dizziness. Others, particularly women, diabetics, elderly, those with dementia, hypercholesterolemia and no family history of heart disease, may present with atypical symptoms. Atypical symptoms are those that are not typical, can be sharp chest pain, may only be associated symptoms or discomfort not located in the chest (i.e., arms, epigastrium, shoulder, neck). In one study, 65% of women presented with atypical symptoms. Elderly, obese, and diabetics also present with atypical symptoms at higher frequencies.
2. In a patient with modifiable risk factors for ischemic heart disease (e.g., smoking, diabetes control, obesity), develop a plan in collaboration with the patient to reduce her or his risk of developing the disease.
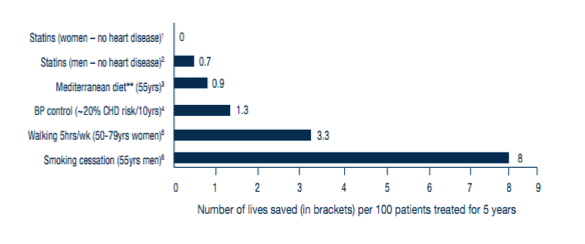
Modifiable risk factors for IHD include obesity, smoking, hyperlipidemia, diabetes, poor glycemic control, hypertension/ uncontrolled HTN and sedentary lifestyle. Plan patients about their risk and assessment of RF as above to calculate a Framingham score. Early diagnosis and treatment of HTN and diabetes is highly beneficial. Effect of blood lipid control in primary prevention remains controversial, especially as it pertains to women and the elderly.
Smoking cessation: Educate, evaluate , medical interventions. Refer to QuitNow.
Physical activity: Give Rx, 30min OD at intensity no sing but talk, 15min resistance 3/wk.
Weight reduction: BMI below 27 is recommended Weight loss.
Dietary recommendations: fish, fruits, fiber, fresh vegetables, low-fat
3. In a patient presenting with symptoms suggestive of ischemic heart disease but in whom the diagnosis may not be obvious, do not eliminate the diagnosis solely because of tests with limited specificity and sensitivity (e.g., electrocardiography, exercise stress testing, normal enzyme results).
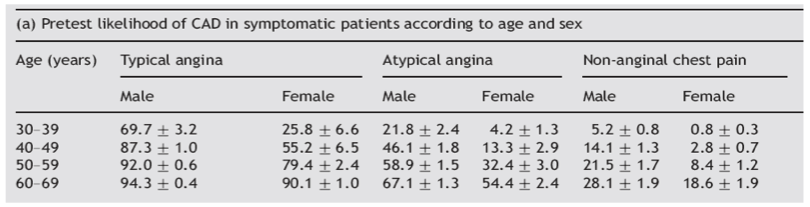
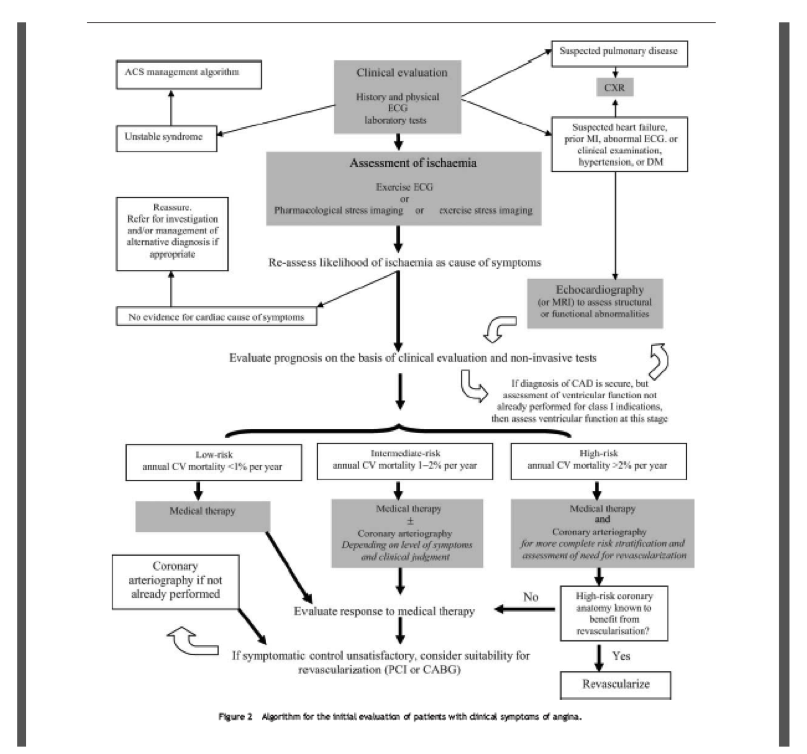
In majority of cases, dx of IHD can be made on Hx and Px but objective test should be used to add or subtract from the pretest probability. Testing should begin with calculation of pretest probability of disease, and then appropriate test designated.
ECG- minimal diagnostic value
Resting ECG must be done on all patients but it has no utility for ruling out IHD. However, a previous MI, LBBB, PRWP, T wave changes, or axis deviation may add to pretest probability but by no means is it diagnostic. ECG during pain episodes may however show ST changes supporting IHD diagnosis. Also presence of BBB or WPW disqualifies patients for stress ECG testing.
Stress ECG testing- ideal for patients with intermediate pretest probability.
Sensitivity for IHD is 68% and specificity is 77%, therefore not ideal for ruling out disease. In patients with high pretest probability this is not ideal diagnostic choice since high false negative may lead to ignoring of the clinical findings. However, this test may be done for prognostication. Angiography is warranted if there is severe stable angina with a high pre-test probability of disease
In low probability group, controversy remains. A negative test decreases the probability but a positive test will then require further testing.

The sensitivity and specificity of non-invasive stress ECG is even poorer in women. However, no consensus on whether directly advancing to imaging techniques with higher sensitivity and specificity exists.If contraindications to stress ECG or dx still in doubt, exercise echo or MIBI which provide higher sensitivity and specificity should be undertaken.
4. In a patient with stable ischemic heart disease manage changes in symptoms with self-initiated adjustment of medication (e.g., nitroglycerin) and appropriate physician contact (e.g., office visits, phone calls, emergency department visits), depending on the nature an severity of symptoms.
All patients should be given sublingual or spray NTG or chewable nifedipine and instructed in its use. Anginal discomfort that lasts >2 or 3 minutes should prompt the patient to discontinue the activity or remove himself or herself from the stressful event. If pain does not subside immediately, the patient should be instructed to take NTG. If the first tablet or spray does not provide relief within 5 minutes, then a second dose, at 5-minute intervals, should be taken. Pain that lasts >15 to 20 minutes or persistent pain despite 2 NTG doses should prompt the patient to seek immediate medical attention by calling 9-1-1 and going to the nearest hospital ED, preferably by ambulance or the quickest available alternative. If the pattern of anginal symptoms changes (eg, pain that is more frequent or severe, is precipitated by less effort, or now occurs at rest), the patient should contact his or her physician to determine the need for additional treatment or testing.
5. In the regular follow-up care of patients with established ischemic heart disease, specifically verify the following to detect complications and suboptimal control:
- symptom control.
- medication adherence.
- impact on daily activities.
- lifestyle modification.
- clinical screening (i.e., symptoms and signs of complications).
6. In a person with diagnosed acute coronary syndrome (e.g., cardiogenic shock, arrhythmia, pulmonary edema, acute myocardial infarction, unstable angina), manage the condition in an appropriate and timely manner.
Patients presenting with prolonged (> 10 minutes) acute chest pain suggestive of ACS require a history and physical examination. If a patient presents in a physician’s office or walk-in clinic and no alternative cause can be found with certainty, referral of the patient to the Emergency Department (ED) for further evaluation and observation is essential. If a previous electrocardiogram (ECG) is available, send it with the patientAdmit and immediately treat patients with a history and ECG (without ST segment elevation) compatible with ischemia, plus either elevated cardiac biomarkers (>99th percentile) or hemodynamic compromise (hypotension or electrical instability), for acute myocardial ischemia or patients with new ST segment elevation or new LBBB and a history compatible with ACS, with the intent of re-establishing perfusion.
Management of patients with possible ACS
It is recommended that patients with a compatible history and a non-diagnostic initial ECG and cardiac biomarkers, be observed in the ED and be re-assessed at six or more hours after the initial testing with an ECG and cardiac biomarkers and exam for hemodynamic changes.For low-risk patients without an obvious alternative explanation for the chest pain an out-patient stress test within 72 hours and out- patient physician follow-up is recommended. For Intermediate-risk patients a stress test prior to discharge is recommended.