Documentation:FIB book/Measurement tools for traumatic brain injuries sustained in ice hockey
Overview
Introduction
There is a high prevalence of concussions, also referred to has minor traumatic brain injury (mTBI)[1], in high-speed contact sports, including ice hockey. Protective helmets primarily reduce concentrated loading and accelerations that cause skull fractures but are not 100% effective in preventing concussions[2]. Ice hockey can be a high-velocity sport that involves both intentional and non-intentional body contact with other players, as well as the boards of the ice rink. Due to the random nature of the sport, various mechanisms can cause head injury resulting in mTBI, either in games, or practice. In recent years, the importance for investigating head impacts has increased. To better understand the mechanisms, and injury tolerances producing concussions, the various methods for measuring impacts are further discussed in this review.
Background
Concussion and Minor Traumatic Brain Injury (mTBI)
The word concussion in Latin literally means to violently shake something[3]. For the purposes of this review, the terms concussion and mTBI can be used interchangeably, however there is controversy related to this topic. Within this review, an mTBI can be defined as a “trauma-induced disturbance”[3] applied to the head or body, resulting in neurological impairment. The symptoms of mTBI a physician can adequately diagnose include balance impairment, behavioral changes, cognitive dysfunction, and sleep/wake disturbance, headache, amnesia, neurologic deficits[3].
During impact or trauma, the brain experiences two types of acceleration: linear and rotational. Of the two acceleration types, the presence of rotational acceleration increases the likelihood of sustaining a mTBI[3] as it is more detrimental than linear acceleration. Linear acceleration typically generates pressure within the skull and waves that propagate intracranially, whereas rotational acceleration induces a shearing force in the brain tissues[3]. This shearing force transfers more energy into the deep tissues of the brain, causing more severe damage[4].
MTBI can have detrimental effects on neurologic function, however, are difficult to diagnose as they are not commonly detected using current imaging modalities[3]. Symptoms can vary physically, emotionally, or cognitively, including loss of consciousness, amnesia, personality of behavior changes, emotional liability, and/or delayed motor and verbal responses[1][3]. Other long term side effects of mTBI include early onset Alzheimer’s and chronic traumatic encephalopathy[1].
Prevalence of mTBI in Ice Hockey
In ice hockey, players play in different positions, defensive, forward, or goalie. Forwards sustain a considerable number of more impacts than defensive players; of the two types of forward positions, wingers are more likely to sustain a higher number of traumatic impacts compared to players playing as a center[5]. This is due to the nature of what each position is responsible for in terms of gameplay. Defensive players typically remain in the low corners of their end of ice (defensive zone), whereas wingers typically play in the corners of the offensive zone. Forwards can be more aggressive in the offensive zone as their “job” is to increase offensive chances in scoring a goal, placing them in the corners and along the boards more often[5]. Additionally, they can take more hits and body contact from opposing players as they are trying to prevent a goal from being scored, increasing the likelihood of head-contact occurring with the players or the boards.
Not only do plays along the boards or impacts with other moving players cause traumatic brain impacts, but higher levels of hockey allow fighting, increasing the odds a player has of sustaining mTBI. A study documented 223 impacts per season in high school aged ice hockey players, and between 170 and 347 impacts in collegiate level players[6]. Furthermore, the average impacts found in a study on Bantam* youth hockey players concluded that the average impact acceleration was 20g, a similar measure to collegiate level football players in America[5]. The development of cognitive function is at its peak in youth[5], and further investigation into the levels of trauma the brain experiences from head impacts in ice hockey is required to determine prevention mechanisms for mTBI.
* Bantam hockey age ranges vary between male and female leagues. Bantam boys’ hockey includes ages 13-15 (15U), and bantam girls’ hockey includes ages 14-16 (16U).
Measurement Techniques
Developing ways for understanding traumatic brain injury date back as far as the early 1900’s[7]. Military surgeon, Jean-Pierre Gama, created an early model comprised of a spherical flask and isinglass matrix fine glass threads to model the skull and brain tissues, respectively[3]. When the flask was tapped from the side, the threads inside oscillated, helping with visualization of the shear force strain within the tissues upon impact[3]. Since this early model, various measurement tools have been developed to better understand the mechanisms of traumatic brain injury including video-based methods and various wearable sensors. These measurement methods are necessary, as they provide an alternative to conducting randomized controlled trials (RCTs) that use concussions in subjects as endpoints[2]. RCTs observe large numbers of subjects during sport-impact situations over a long period of time. They are resource intensive and lengthy. In contrast, quantifying impact kinematics with measurement methods could be a more efficient way to study brain injury during sport.
Helmet-based Measurement Systems

Helmet-based measurement systems have been widely used in sports, including hockey[5][8]. The helmet-based measurement system uses accelerometers in helmets to measure the linear and rotational acceleration during an impact. The most used helmet-based system for sports is the head impact telemetry (HIT) system[8]. The HIT system combines hardware and software to detect and record the impact[9]. The hardware component uses six single axis accelerometers inside a helmet to measure the impact[6]. While some systems attach the sensor from the outside of the helmet (e.g. Shockbox Hockey Helmet Sensor, Gridiron tec), HIT system embedded the accelerometers in the helmet[8]. Since many sports such as hockey require the players to wear helmets, such a system is relatively easy to implement. According to one study[6], the system will record data between 8 ms prior to the impact and 32 ms after the impact with a sampling rate at 1 kHz. Helmet-based systems will filter out impacts with peak accelerations lower than 10g and calculate resultant angular velocity using regression-based algorithms[6].
Skin Patches
Skin patch systems attach the sensor directly to the skin, usually behind the ear, to measure the acceleration of the head during an impact. Skin patch systems can be used in both helmeted or non-helmeted sports and are a more cost-effective wearable sensor in comparison to the HIT system[10]. According to a recent systematic review, X-Patch (X2 Biosystems, Inc) is the most widely studied skin patch sensor for head impact measurement[6]. The sensor has six degrees of freedom, with a triaxial accelerometer and gyroscope to measure the linear and angular acceleration[6]. The sampling rate of the X-Patch is 1 kHz for the resultant linear acceleration and around 850 Hz for resultant rotational acceleration[6]. The sensor will record data from 10 ms before the impact to 90 ms after the impact[6]. According to the review[11], by using the X-Patch sensor, concussion-related head impacts decreased by 30 to 70% in adolescent and professional sports, likely due to the improvement in safety measures. For example, in soccer, coaches can use this data to help determine whether a player has sustained a large impact, which requires removal from the game.[12].
Instrumented Mouthguards (iMGs)
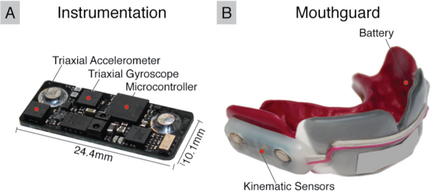
Instrumented mouthguards (iMGs) are mouthguards instrumented with inertial sensors. They include a triaxial accelerometer and angular accelerometer/gyroscope to measure linear and angular kinematics in three degrees of freedom. This is a practical option for contact sports such as hockey, as players often wear mouthguards in practice and in competition. This technology has been developed to improve skull coupling so that skull kinematics can be measured more accurately.
A recent study showed that iMG data of peak linear and angular kinematic accelerations agreed well with reference data measured on a dummy headform[13]. Reference sensors can be rigidly attached to the skull centre of gravity (COG) of the dummy head during these laboratory tests. Therefore, sensor accuracy can be evaluated without having soft tissue motion affect the results[14]. The study assessed four current instrumented mouthguards (Biocore-Football Research Inc (FRI)[15], HitIQ[16], ORB Smartguard [17], Prevent IMM [18]). Table 1 lists product specifications for these four mouthguard sensors in the study[13]. The headforms were impacted at various locations, impact magnitudes and durations using a pendulum impactor. The different magnitudes corresponded to target head linear accelerations of 25g, 50g, 70g, and 100g. The duration of impact was varied by changing the headform padding (headform paddings: rigid head, nylon 25 mm thickness and padded, vinyl-nitrile foam 40 mm thickness). The custom-fit iMGs were mounted inside the headform mouth to measure impact kinematics and were compared with the reference kinematics[13].
| Instrumented Mouthguard (iMGs) | ||||
|---|---|---|---|---|
| Biocore-FRI | HitIQ | ORB | Prevent | |
| Linear sampling rate (Hz) | 5500 | 3200 | 1600 | 3200 |
| Angular sampling rate (Hz) | 5500 | 800 | 1600 | 3200 |
| Output time window (ms) | 71
(21 ms pre-trigger; 50ms post-trigger) |
100
(20ms pre-trigger; 80ms post-trigger) |
100
(51ms pre-PLA peak; 49ms post-PLA peak) |
50
(10ms pre-trigger; 40ms post-trigger) |
The measurements from three of the iMGs (Biocore-FRI, HitIQ and Prevent) had a linear and angular mean bias of within 7%[13]. They also had a close linear relationship with the reference values (total correlation coefficient values > 95%)[13]. This was higher than any other wearable head sensors previously evaluated in similar laboratory tests[13].
Other Wearables
In addition to the wearable sensors discussed above, other forms of sensor attachments including headbands (e.g. Sim-G; Triax Technologies, Inc) have also been studied. In addition, skullcaps have also been a good alternative (e.g. SmackCap; Pressure Analysis Company). Although these are some more economical and convenient options, these sensors are not attached to the head as firm as the helmet or skin patch system, which results in a larger error[10]. Moreover, some other researchers have been working on using sensors other than head accelerometers and gyroscopes to measure head impact[19]. For example, one study proposed a head impact monitoring system with which eye movement is used to determine the brain trauma[19].
Skull Coupling of iMGs vs. Other Sensor Types
One reason for the inaccuracy of skin patches and other helmet/headgear mounted sensors when measuring head kinematics is due to poor skull coupling. One study evaluated sensor coupling to the skull of a custom-fit instrumented mouthguard developed by the research team, a skin patch sensor (xPatch Gen2, X2Biosystems, Inc), and elastic skull cap sensor (Reebok) in a human subject during mild soccer head impacts[14]. The relative displacement of each sensor from a deeply inserted ear plug was tracked through high-speed video to evaluate skull coupling. This was appropriate, as the bony part of the ear canal is very well coupled to the skull.
All 16 head impact trials for the mouthguard showed displacements within the video measurement error of <1 mm (µ = 0.5 mm, σ = 0.2 mm)[14]. To reduce decoupling from soft tissue, the skin patch was mounted on the mastoid process behind the ear. Despite this, the skin patch sensor displaced by 2 mm to 4 mm (µ = 3 mm, σ = 0.7 mm), and the skull cap sensor displaced by 2 mm to 13 mm (µ = 5 mm, σ = 3 mm)[14]. Since the mouthguard demonstrated the best skull coupling, its kinematic measurements in 6 degrees of freedom were used as a reference to compare with the measurements from the other two sensors. Skin patch estimation of head linear and angular acceleration peak values were over-predicted by 15 ± 7g and 2500 ± 1200 rad/s2 on average. The skull cap values were overpredicted by 50 ± 31g and 4300 ± 2700 rad/s2[14]. The skin patch and skull cap measurements were not linearly correlated with the mouthguard reference measurements; generally, they exhibited a random relationship with the reference. In addition, the skull cap and skin patch sensors did not accurately predict the direction of head motion that was seen on film. This out-of-plane motion contributed to the over-prediction in skull kinematics[14]. The skin patch measured a significant amount of left-right translation and horizontal rotation of the head. The skull cap had highly variable directionality of kinematic data. In contrast, the mouthguard accurately predicted the direction of rotation in the sagittal plane, with anterior-posterior translation, which is expected in a frontal soccer heading.
Controversies in Research
There is an abundance of work detailing head injuries and mTBI, as well as measurement tools and preventative technologies. Due to the large amounts of information regarding traumatic brain injuries, controversies between different research groups and findings have emerged.
Definition of Traumatic Brain Injury
Controversy between many studies relates to the definition of an mTBI, it’s interchangeable use in terminology with concussion[3] [20], as well as diagnostic criteria and medical management[3]. Additionally, traumatic head impact can produce loss of consciousness, however not all impacts have this effect, and the degree of loss of consciousness varies based on grade of concussion[3]. The nature of variability in head trauma can lead to differences in post-impact symptoms at similar levels of neurological injury [20], further contributing to controversy over what defines an mTBI.
Methods of Impact Measurement
A manuscript [21] argued the methods and conclusions in a helmet-based sensor study[8] were invalid and misleading, with the impact rates published in the study being overestimated. The manuscript claims the helmet fit used in the study[8] was unsatisfactory and unrealistic of real-world conditions due to a lack of chin strap attachment, and improper fit of the chin pad to the headform [21]. Additionally, the impact delivery methods used in the study[8] – a spherical impactor ram – do not properly simulate on ice head impacts with a flat surface like the ice surface or boards, or another player’s head [21].
In addition to the above controversy, a common disagreement that exists in academia is related to error produced from the different methods of measurement[3][14][22]. In one study, discrepancies between skull cap and mouthguard measurements was discussed, with skull cap sensing methods producing HIC values of higher than 250 and the wearable mouthguard producing HIC values of 1.3 ± 0.6 for the same impact events[3][14]. A HIC value of 250 has been cited as the concussion threshold[23].
The study also compared the accuracy of skin patches to head mounted sensors, again observing higher measured HIC values for the skull cap, and overall overestimation of brain injury criterion[24] for both methods[14]. These discrepancies are likely due to the lack of coupling tools that a skin patch or cap can provide with the skull. Sensors mounted or embedded in a mouthguard offer the potential to maximize accuracy in measurement of the kinematics of the head as they have tighter coupling with the skull[2].
Limitations of Research
Although there is an abundance of research detailing different methods in which head impact can be measured, there are a variety of limitations that are inherent in head impact research. The limitations that arise stem from current efforts to quantify the innate complexities of head impacts.
Helmeted Devices
The accuracy of measurements taken by helmeted devices is greatly influenced by the location of impact. In most cases, the most accurate measurements are obtained from frontal impacts, while impacts that occur at the crown of the head are less accurate[6]. In addition, some impacts that hit other parts of the body may not exceed the helmet sensor threshold but still have consequences on the brain[22][25]. The head impact telemetry system (HITS) is an analysis tool that uses device measurements to estimate head injury severity[6]. However, this system assumes that the helmet and skull move as a single rigid body - thus, the accuracy of this analysis is significantly dependent on the appropriate fit of the helmet. Helmeted devices that are instrumented with spring loaded accelerometers must maintain continuous contact with the skull to accurately measure the acceleration and deformation of the skull during impact. As detailed in a systematic review, the HITS analysis tool produced error ranges from 7-18% for resultant linear acceleration and 12-27% for resultant angular acceleration[6].
Non-helmeted Devices
Non-helmeted devices have inherent limitations as well. Regarding skin patches, accuracy is greatly dependent on adherence to the skin and can be negatively influenced by skin motion[6]. Measurement accuracy of headbands and skull caps are significantly affected by attachment as well[10]. Mouthguard sensors are expensive, and their accuracy is significantly affected by the fit of the mouthguard as well as saliva accumulation. In general, non-helmeted devices are greatly limited by the size of the device, as such the sensors that are used must be relatively small as well. Because of this, errors are most significant in short duration impacts due to their low sampling rate[10]. Furthermore, the filtering algorithms that are used to analyze the data obtained can further decrease the accuracy of the data.
The accuracy of X-Patch system has been examined by multiple studies[10][26][27]. For example, one study examined the accuracy of this sensor with a Hybrid III head form[27]. With 400 impact tests, the sensor showed 24% error in linear acceleration and 57% error in angular acceleration[27]. They also noted that the location of the impact may significantly affect the detection results[27]. Significant error is observed in other laboratory tests, which has a more consistent environment and no other factors, such as sweating and face movement, affecting the measurement[10]. Due to the sampling rate limit, a large error can be seen in short impact time events, for example, an impact with a ball that has a high stiffness[26].
False Positives & Video Verification
Another prevalent limitation to the aforementioned measurement techniques is the overwhelming number of false positives that are observed in studies that measure head kinematics during sports competition. Sensors that are instrumented into the measurement devices start recording the impact after reaching a defined acceleration threshold[6]. In ice hockey, there are many sources of non-head impacts that may cause the sensors to exceed the recording threshold and as such, false positive measurements are very common. Researchers have attempted to combat this limitation by matching triggered events to video recordings of players in order to verify positive readings[10][22]. Although this method mitigates part of the problem, researchers were unable to verify some instances of head impact due to an obstructed view of the players. Furthermore, cross-referencing footage of players is an extremely time-consuming process, taking over 1000 cumulative hours to analyze seven players[22]. Because of this, video analysis is not a feasible solution for large sample sizes and data sets.
General Big-Picture Limitations
In general, although head-impact sensors may provide valuable information to researchers and sideline staff, they currently have limited applications to concussion diagnosis. Given the current state of technology and the previously discussed limitations of equipment, head-impact data can only be used to provide context about the accelerations that the athlete underwent during the impact. As this data is more objective compared to video analysis or self-reported experience, the data can only be used as supplementary information for clinicians to make quicker and more accurate diagnoses[6].
Recommendations and Future Work
Unanswered Questions
Engineers and clinicians still do not understand the exact relationship between head kinematics and the risk of attaining an mTBI[2]. Even with very accurate head impact kinematic measurements, it might still be difficult to evaluate injury risk. When the head undergoes angular accelerations, the brain moves independently within the skull cavity and deforms[6]. Simulating the stresses and strains in the brain during impact scenarios through computational models could provide a more direct measure of brain injury risk[2]; however, this is only possible if accurate data from inertial sensors are used as inputs to drive these models.
Future work
The focus of future work should be to gather large amounts of accurate kinematic and injury data from impact events during real hockey games. This data can then be used to simulate brain tissue deformation with computational models. The data collected could then be applied to create an injury risk criterion for concussions and improve concussion treatment, diagnosis, and the design of better protective equipment for hockey athletes[2].
It is difficult to replicate all possible scenarios that could lead to head acceleration events in hockey players during laboratory testing. Once sensors are validated in the lab, they should be used in studies that measure kinematics during games.
As detailed in this literature review, iMGs performed the best of all wearable sensor types in laboratory testing and present the least number of limitations. These sensors exhibit the most potential for accurately measuring head kinematics during in-game hockey impact events. Assessing the validity of iMG-triggered head acceleration events during these studies by identifying true-positives, false-positives and false-negatives via video verification will be crucial. However, as previously discussed, cross referencing footage of players is an extremely time-consuming process[22]. Methods that utilize machine learning algorithms could be developed to automate this process. While instrumented mouthguards offer superior skull coupling over other wearable sensors, they still cannot directly measure brain movement, due to the free movement of the brain in the skull cavity[6]. Thus, it might be necessary to investigate novel forms of sensors that do not rely on tracking skull motion, such as eye trackers.
References
- ↑ 1.0 1.1 1.2 C. S. Sahler and B. D. Greenwald, "Traumatic Brain Injury in Sports: A Review," Rehabilitation Research and Practice, vol. 2012, pp. 1-10, 2012.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 L. Wu, "Sport Concussions: can head impact sensors help biomedical engineers design better headgear?," British Journal of Sports Medicine, 2019.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 S. E. Chancellor, E. S. Franz, O. V. Minaeva and L. E. Goldstein, "Pathophysiology of Concussion," Seminars in Periatric Neurology, vol. 30, pp. 14-25, 2019.
- ↑ A. K. Ommaya and T. A. Gennarelli, "Cerebral concussion and traumatic unconsciousness. Correlation of experimental adn clincal observations of blunt head injuries," Brain, vol. 97, pp. 633-654, 1974.
- ↑ 5.0 5.1 5.2 5.3 5.4 N. Reed, T. Taha, M. Keightley, C. Duggan, J. McAuliffe, J. Cubos, J. Baker, B. Faught, M. McPherson and W. Montelpare, "Measurement of Head Impacts in Youth Ice Hockey Players," Orthopedics and Biomechanics, vol. 31, pp. 826-833, 2010.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 K. L. O'Connor, S. Rowson, S. M. Duma and S. P. Broglio, "Head-impact - measurement devices: A systematic review," Journal of Athletic Trainig, vol. 52, no. 3, pp. 206-227, 2017.
- ↑ C. Boake, "A history of cognitive rehabilitation of head-injured patients, 1915 to 1980," Journal of Head Trauma Rehabilitation: September 1989, vol. 4, no. 3, pp. 1-8.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 M. A. Allison, Y. S. Kang, J. H. Bolte 4th, M. R. Maltese and K. B. Arbogast, "Validation of a helmet-based system to measure head impact biomechanics in ice hockey.," Medicine and science in sports and exercise, Vols. 46,1, pp. 115-23, 2014.
- ↑ Wikipedia contributors, "Head impact telemetry system," Wikipedia, The Free Encyclopedia., 27 January 2019. [Online]. Available: https://en.wikipedia.org/wiki/Head_impact_telemetry_system. [Accessed 6 November 2022].
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 A. M. Tyson, S. M. Duma and S. Rowson, "Laboratory evaluation of low-cost wearable sensors for measuring head impacts in sports," Journal of Applied Biomechanics, vol. 34, no. 4, pp. 320-326, 2018.
- ↑ X2 Biosystems, "X-Patch Pro Wearable Sensor," X2 Biosystems Inc, [Online]. Available: https://www.x2biosystems.com/x2_x_patch_pro/. [Accessed 6 November 2022].
- ↑ Fulhamsfinest, "Soccer’s new secret weapon for head-impact safety? The X2 Patch may be it," 18 Feb 2015. [Online]. Available: https://soccer.nbcsports.com/2015/02/18/the-x2-patch-a-new-weapon-for-head-impact-safety-in-soccer/. [Accessed 3 Dec 2022].
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 B. Jones, J. Tooby and D. Weaving, "Ready for impact? A validity and feasibility study of instrumented mouthguards (iMGs)," British Journal of Sports Medicine, no. 56, pp. 1171-1179, 2022.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 14.7 14.8 L. Wu, V. Nangia, K. Bui, B. Hammoor, M. Kurt, F. Hernandez, C. Kuo and D. Camarillo, "In Vivo Evaluation of Wearable Head Impact Sensors," Annuls of Biomedical Engineering, vol. 44, no. 4, pp. 1234-1245, 2016.
- ↑ Biocore, "Biocore," 2022. [Online]. Available: https://biocorellc.com/#mouthguard-sensors. [Accessed 3 December 2022].
- ↑ HitIQ, "Measure, manage and mitigate head impacts," 2022. [Online]. Available: https://hitiq.com/product. [Accessed 3 December 2022].
- ↑ ORB Innovations, "ORB Smartguard," 2022. [Online]. Available: https://www.orbinnovations.com/. [Accessed 3 December 2022].
- ↑ P. Biometrics, "How it Works," 2022. [Online]. Available: https://preventbiometrics.com/the-system/. [Accessed 3 December 2022].
- ↑ 19.0 19.1 J. C. Prather, Y. Meng, M. Bolt, T. Horton and M. Adams, "Wireless head impact monitoring system utilizing eye movement as a surrogate for brain movement," AEU - International Journal of Electronics and Communications, vol. 105, pp. 54-61, 2019.
- ↑ 20.0 20.1 R. Romeu-Mejia, C. C. Giza and J. T. Goldman, "Concussion Pathophysiology and Injury Biomechanics," Current Reviews in Muskuloskeletal Medicine, vol. 12, pp. 105-116, 2019.
- ↑ 21.0 21.1 21.2 B. J. Wilcox, J. G. Beckwith, R. M. Greenwald and J. J. Crisco, Limitations of "validation study of helmet-based impact measurement system in hockey", vol. 46, Med Sci Sports Exercise, 2014, pp. 640-641.
- ↑ 22.0 22.1 22.2 22.3 22.4 C. Kuo, L. Wu, J. Loza, D. Senif, S. C. Anderson and D. B. Camarillo, "Comparison of video-based and sensor-based head impact exposure," PLOS One, vol. 13, no. 6, pp. 1-19, 2018.
- ↑ E. L. Pellman, D. C. Viano, A. M. Tucker, I. R. Casson and J. F. Waeckerle, "Concussion in Professional Football: Reconstruction of Game Impacts and Injuries," Neurosurgery, vol. 53, no. 4, pp. 799-814, 2003.
- ↑ E. G. Takhounts, M. J. Craig, K. Moorhouse, J. McFadden and V. Hasija, "Development of brain injury criteria (BrIC)," National Library of Medicine, vol. 57, pp. 243-266, 2013.
- ↑ N. Cortes, A. E. Lincoln, G. D. Myer, L. Hepburn, M. Higgins, M. Putukian and S. V. Caswell, "Video Analysis Verification of Head Impact Events Measured by Wearable Sensors," The American Journal of Sports Medicine, vol. 45, no. 10, pp. 2379-2387, 2017.
- ↑ 26.0 26.1 D. Nevins, L. Smith and J. Kensrud, "Laboratory evaluation of wireless head impact sensor," Procedia Engineering, vol. 112, pp. 175-179, 2015.
- ↑ 27.0 27.1 27.2 27.3 S. Tiernan, G. Byrne and D. M. O'Sullivan, "Evaluation of skin-mounted sensor for head impact measurement," Proceedings of the Institution of Mechanical Engineers. Part H, Journal of engineering in medicine, vol. 233(7), p. 735–744, 2019.