UnderstandingMiscarriages
Introduction
Miscarriage, also known as pregnancy loss, spontaneous abortion, or stillbirth, is tremendously common. In fact, between 22 and 89% of all pregnancies are believed to end in a miscarriage, with roughly two out of three miscarriages occurring before a woman is aware she is pregnant.[1] To put this into perspective, heart disease kills one in four Americans, cancer kills nearly twice as many, and strokes kill about one in twenty. Miscarriage is unquestionably deadlier than any of these, possibly deadlier than all of these combined.[2]
Here is a very informative YouTube video that provides a great overview on miscarriages[3] https://www.youtube.com/watch?v=_ojUPrxRGgQ
Definition
Miscarriage can be defined as the loss of pregnancy before 24 completed weeks’ gestation. An alternative definition is a pregnancy that fails to proceed, triggering the death and removal of the embryo or fetus weighing 500g or less. On occasion, a baby may be born alive at less than 24 completed weeks of gestation. This type of pregnancy is referred to as a live birth and if the baby does not survive, it is then termed a neonatal death.[4]
Signs and Symptoms

Bleeding
Vaginal bleeding is normally the first sign of a miscarriage, but it may be misleading. Approximately 30% of women have bleeding during their pregnancies, nevertheless, not all of them will miscarry.[5]
Pain
The pain may be situated in the abdomen, pelvic area, or lower back. It may range from dull and sore to period-like cramping.[6] Painful contractions occurring 5 to 20 minutes apart may indicate premature labor.[7]
Change in pregnancy symptoms
A decrease in pregnancy related symptoms such as nausea, vomiting, weight gain, or breast tenderness may indicate a miscarriage. An abrupt change before the second trimester may suggest a decrease in pregnancy hormones.[8]
These symptoms do not always mean a woman will have a miscarriage. A woman may exhibit some of these symptoms but still have a healthy pregnancy. Still, a miscarriage may occur without any symptoms at all; this is known as a missed miscarriage.[9][10]
Causes
Chromosomal abnormalities
Chromosomal abnormalities are the main causes of miscarriages. These occur when the sperm and egg come together but one of them has too many or too few chromosomes. In other cases, the 23 pairs of chromosomes from each parent fail to line up correctly. Whichever way, the embryo isn’t hereditarily tough enough to withstand a viable pregnancy.[11]

Medical disorders
Chronic medical conditions and autoimmune diseases such as blood clotting disorders, thyroid disease, diabetes, and lupus can result in a miscarriage or affect pregnancy.[12]
Uterine abnormalities
A uterine septum or any anatomic irregularities are responsible for roughly 10% of recurrent miscarriages. Another possible cause is an incapable or weakened cervix. Generally, during pregnancy, the cervix, the lower part of the uterus that attaches to the vagina, is closed and inflexible. However, in this case it starts to open too early and can result in a miscarriage.[13]
Risk Factors
- Age. Women older than 35 have a higher risk of miscarriage than do younger women[14]
- Previous miscarriages. Women who have had two or more consecutive miscarriages are at higher risk of miscarriage[15]
- Smoking. Smoking can reduce the oxygen to the baby and cause chromosomal abnormalities in pregnancy[16]
- Caffeine. Higher levels of caffeine play a part in pregnancy loss[17]
- Alcohol. Drinking can cause fetal alcohol effects or severe fetal alcohol syndrome[18]
- Weight. Being underweight or being overweight pre-pregnancy has been linked with an increased risk of miscarriage[19]
- Diet and behaviour. Taking vitamins, eating fresh fruit and vegetables, and consumption of dairy products and chocolate decreases the risk of a miscarriage[20]
- Father. There is an increased risk of miscarriage when the father is aged older than 45 years. Also, Women who conceive after a change in partner have a 60% increase in the odds of miscarriage than women who do not switch partners[21]
Diagnosis
The most common way that a miscarriage is diagnosed is through an ultrasound. Some features looked for are remains of conception, such as villi, and fetal parts such as the amniotic sac and the embryo.[22] The criteria include:

- Empty sac: no noticeable embryo in the womb[23]
- Embryonic or fetal loss: no cardiac activity in the embryo[24]
- Delayed miscarriage: decrease in cardiac functions; delay of the foetal size; no visible embryo (empty sac) at 12 weeks of gestation[25]
- Complete miscarriage: no remains of conception or uterine products; whereabouts of the pregnancy are unknown; ectopic pregnancy[26]
- Incomplete miscarriage: cervix is opened and there are remains of irregular pieces of conception still inside the uterus[27]
- Heartbeat: an ultrasound can detect whether or not the baby has a heartbeat[28]
Treatment
Observation/expectant management
Some women prefer to let the miscarriage occur naturally. Typically, the miscarriage will pass within 2 weeks. It is important to watch for signs of infection (fever, chills, feeling sick) or heavy bleeding.[29]
Medication
Medication can help the body pass the miscarriage. It can either be taken by mouth or put in the vagina and generally works within 24 to 48 hours. Heavy bleeding and cramping is expected.[30]
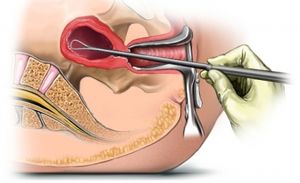
Surgery
Surgery is a common treatment for a miscarriage and is a popular choice after other methods of treatment fail to work. The usual surgery is a D&C (dilatation and curettage). A small suction device is positioned in the uterus (womb), and the pregnancy is removed. With this surgery comes a small chance that that the lining of one’s uterus can be damaged, and one might have difficulty getting pregnant again.[31]
Induction of labor
If the pregnancy lasted greater than 16 weeks, one may be admitted to the hospital to induce labor. This is often a lengthy process that may comprise the use of several different medicines.[32]
After a miscarriage
After a miscarriage, it is best not to bottle up feelings but to discuss them as fully as possible with anyone else who can listen and understand.[33] Hospitals and community agencies offer support programs that can provide follow-up care and information. [34]
References
- ↑ Simpson, J. L. (2011). Early pregnancy loss. In G. Kovacs (Ed.), The subfertility handbook: A clinician’s guide (2nd ed., p. 2011). Cambridge: Cambridge University Press.
- ↑ Berg, A. Philos Stud (2017) 174: 1217. https://doi- org.ezproxy.library.ubc.ca/10.1007/s11098-016-0750-z
- ↑ What is Early Miscarriage – Symptoms, Signs and Causes [Video file]. (2016, July 5). Retrieved October 31, 2017, from https://www.youtube.com/watch?v=_ojUPrxRGgQ
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Brusie, C. M. (2016, February 29). Is It A Miscarriage? The Most Common Symptoms Explained.
- ↑ Brusie, C. M. (2016, February 29). Is It A Miscarriage? The Most Common Symptoms Explained.
- ↑ Showell, B. (n.d.). Miscarriage Symptoms: Signs And Causes. Retrieved October 30, 2017, from https://www.thebump.com/a/miscarriage-symptoms-signs-causes
- ↑ Brusie, C. M. (2016, February 29). Is It A Miscarriage? The Most Common Symptoms Explained.
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ Payne, D. J. (n.d.). Miscarriage. Signs, Symptoms and Causes. Micarriage info. Retrieved October 30, 2017, from https://patient.info/health/miscarriage-and-bleeding-in-early-pregnancy
- ↑ Showell, B. (n.d.). Miscarriage Symptoms: Signs And Causes. Retrieved October 30, 2017, from https://www.thebump.com/a/miscarriage-symptoms-signs-causes
- ↑ Showell, B. (n.d.). Miscarriage Symptoms: Signs And Causes. Retrieved October 30, 2017, from https://www.thebump.com/a/miscarriage-symptoms-signs-causes
- ↑ Showell, B. (n.d.). Miscarriage Symptoms: Signs And Causes. Retrieved October 30, 2017, from https://www.thebump.com/a/miscarriage-symptoms-signs-causes
- ↑ Miscarriage. (2016, July 20). Retrieved October 30, 2017, from https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298
- ↑ Miscarriage. (2016, July 20). Retrieved October 30, 2017, from https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298
- ↑ Robin Elise Weiss, PhD | Reviewed by Anita Sadaty, MD. (n.d.). 9 Risk Factors That Increase Your Chance of Miscarriage. Retrieved October 30, 2017, from https://www.verywell.com/risk-factors-for-miscarriage-2759679
- ↑ Robin Elise Weiss, PhD | Reviewed by Anita Sadaty, MD. (n.d.). 9 Risk Factors That Increase Your Chance of Miscarriage. Retrieved October 30, 2017, from https://www.verywell.com/risk-factors-for-miscarriage-2759679
- ↑ Robin Elise Weiss, PhD | Reviewed by Anita Sadaty, MD. (n.d.). 9 Risk Factors That Increase Your Chance of Miscarriage. Retrieved October 30, 2017, from https://www.verywell.com/risk-factors-for-miscarriage-2759679
- ↑ Miscarriage. (2016, July 20). Retrieved October 30, 2017, from https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298
- ↑ Maconochie, N., Doyle, P., Prior, S. and Simmons, R. (2007), Risk factors for first trimester miscarriage—results from a UK-population-based case–control study. BJOG: An International Journal of Obstetrics & Gynaecology, 114: 170–186. doi:10.1111/j.1471-0528.2006.01193.x
- ↑ Maconochie, N., Doyle, P., Prior, S. and Simmons, R. (2007), Risk factors for first trimester miscarriage—results from a UK-population-based case–control study. BJOG: An International Journal of Obstetrics & Gynaecology, 114: 170–186. doi:10.1111/j.1471-0528.2006.01193.x
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ Bottomley, C., & Bourne, T. (2009). Best Practice & Research Clinical Obstetrics and Gynaecology. Diagnosing miscarriage, 23(4), 463-477. doi:https://doi.org/10.1016/j.bpobgyn.2009.02.004
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ (2013), Miscarriage. Journal of Midwifery & Women's Health, 58: 479–480. doi:10.1111/jmwh.12084
- ↑ Payne, D. J. (n.d.). Miscarriage. Signs, Symptoms and Causes. Micarriage info. Retrieved October 30, 2017, from https://patient.info/health/miscarriage-and-bleeding-in-early-pregnancy
- ↑ Hull, Andrea, and Laura Bennion. Understanding Miscarriage. 23 Vol. Edmonton: Edmonton Journal, 2007. http://search.proquest.com.ezproxy.library.ubc.ca/docview/222691278?pq-origsite=summon