Dietetics:Enteral Nutrition
Disclaimer: The following information is meant for general educational purposes only. All health authorities operate under their specific guidelines and protocols. Therefore, all dietetic students and interns should consult their preceptors and governing health authorities for such information.
Enteral Nutrition Video
This video provides an opportunity for the viewer to work through an enteral case study. It demonstrates the decision making processes involved in enteral nutrition and provides examples of enteral nutrition calculations.
Feeding Tubes and Administration
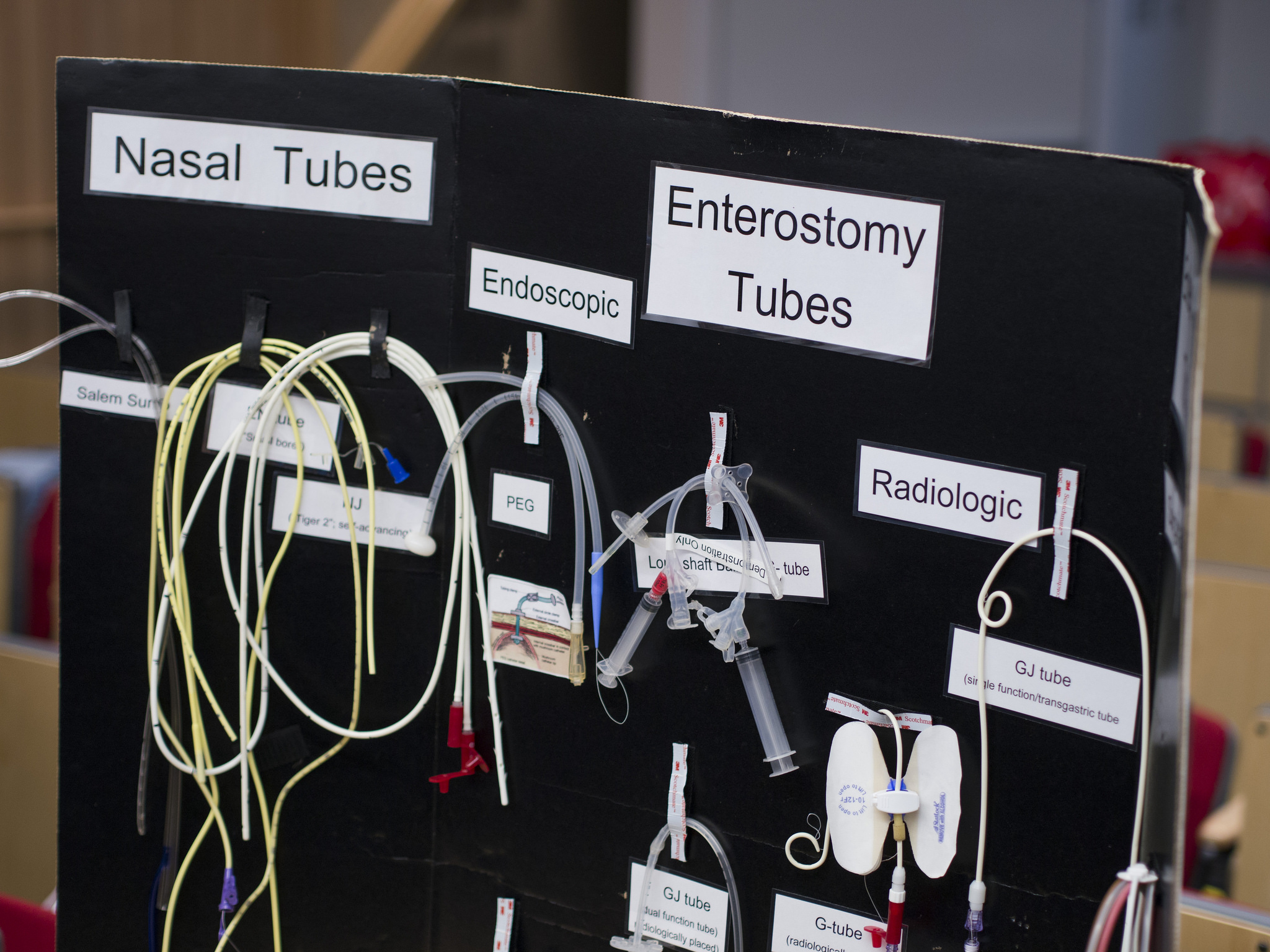
Choosing Feeding Tubes
There are various types of feeding tubes used in enteral nutrition. Some of these include nasogastric, gastric, and jejunostomy tubes. The type of feeding tube chosen should reflect the patient’s nutritional condition and disease state, as well as the expertise of the dietitian and the rest of the health care team.
Considerations for Selecting Feeding Tube and Site of Access
- Patient prognosis and medical condition
- Activities of daily living and quality of life
- Availability of feeding tube experts
- Potential risks associated with different types of feeding tubes and access sites
- Required duration of enteral feeding
Considering the Cost of Feeding Tubes
Feeding tubes need to be changed regularly and for most patients, feeding tubes are not covered under health insurance plans. Therefore, it is important to consider the cost when choosing the correct feeding tube. For example, feeding tubes that are more inconspicuous will cost relatively more compared to a tube that is not.
Feeding Regimens
There are various feeding regimens for enteral nutrition, some of which include bolus, intermittent/cyclic, and continuous regimens, or a combination of these methods. The use of pump or gravity may be chosen for an intermittent feeding regimen, while a pump is typically used in continuous feedings. Administration of enteral nutrition is based on the patient's age, disease condition, nutrition status, and condition of the gastrointestinal tract. The administration rate is usually advanced based on tolerance; however, note that initiating and advancing enteral feeds is guided by clinical judgement and individual institutional practices.
Resources
Enteral Nutrition: How to calculate
Enteral Nutrition Manual for Adults in Health Care Facilities: Pages 14-17
Choosing an Appropriate Formula
Although the enteral formulary of various health care institutions may differ, it is important to become familiar with the categories of formulas that are offered (e.g. standard, hydrolyzed, elemental, disease-specific), and when they may be used. Several of these categories can be found in the Nestle and Abbott product guides.
Factors to Take into Consideration
1. Nutritional Goals
- Will the patient benefit from a disease specific or high protein formula?
- Will the patient benefit from the use of modular formulas (such as Beneprotein)?
- Will the formula be consistent with fluid requirements?
- Is the amount of fibre in the formula appropriate?
2. Digestive and Absorptive Capability
- What is the most intact formula that can be tolerated (e.g. polymeric, hydrolyzed)?
- Is fat malabsorption an issue?
3. Patient Status
- Are there any allergies to be aware of?
- An overview of formulas for certain allergies and diseases: Enteral Formula Selection: A Review of Selected Product Categories
- Are there any medication-formula interactions to be aware of ?
- Do lab values indicate any special needs or restrictions?
- What factors may affect tolerance (e.g. age, infection, GI complications)?
- How long will the patient be using enteral nutrition?
- Will the patient tolerate the odour of the formula?
- Does the patient want to blend their own formula?
4. Cost
- Does the patient have the financial means to access the prescribed formula? (Note: standard, general purpose formulas are typically least expensive)
5. Formula Properties
- Is the viscosity appropriate for the selected feeding tube?
- Will osmolality be well tolerated?
6. Current Best Evidence
- What can be drawn from the current best evidence to guide decisions (e.g. evidence regarding supplemental arginine/glutamine/antioxidants)?
- Summary of evidence from Canadian Clinical Practice Guidelines
Resources
BC Children's Hospital: Types of Tubes
Nutrition411: Feeding Tube Types
Dietitian.org: The Selection and Care of Enteral Feeding Tubes