Course:COGS200/2017W1/Group25
A Combined Virtual Reality Electroencephalography Head Mount Display as a Suitable Rehabilitation Alternative to Treatments Currently Available for Patients Suffering from Post-Traumatic Stress Disorder.
Introduction
Introduction to Post-Traumatic Stress Disorder (PTSD)
The term “trauma” is understood to refer to an event that involves witnessing or being a victim of an act of violence, atrocity, or death of another individual or the near death of one’s self. Traumatic events are inevitable in today’s society and it is believed that an estimated 70% of Americans experience a traumatic event sometime within their lifespan, and 20% of that population go on to develop a form of Post-Traumatic Stress Disorder (PTSD) (National Center for PTSD, 2017). Unfortunately over the years, the general public and health professionals have been skeptical as to whether or not PTSD was a real disorder. It was only in 1980 that PTSD was recognized by the American Psychiatric Association as a psychobiological mental disorder with specific symptoms that could be diagnosed, and the disorder was added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Although PTSD is mainly thought to affect military veterans, it is not limited to combat experience and can have effects on victims of natural disasters, terrorist attacks, serious accidents, and sudden or major emotional losses. It is also twice as prevalent in woman than in men as they are more likely to experience a form of sexual or physical assault (National Center for PTSD, 2015).
DSM-5 Criteria for Diagnosis
The American Psychiatric Association’s (2013) DSM-5 requires the following eight criteria to be present or met in order for a patient to be diagnosed with PTSD:
- Criterion A: stressor
- The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, as follows: (one required)
- i. Direct exposure.
- ii. Witnessing, in person.
- iii. Indirectly, by learning that a close relative or close friend was exposed to trauma. If the event involved actual or threatened death, it must have been violent or accidental.
- iv. Repeated or extreme indirect exposure to aversive details of the event(s), usually in the course of professional duties (e.g., first responders, collecting body parts; professionals repeatedly exposed to details of child abuse). This does not include indirect non-professional exposure through electronic media, television, movies, or pictures.
- The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, as follows: (one required)
- Criterion B: intrusion symptoms
- The traumatic event is persistently re-experienced in the following way(s): (one required)
- i. Recurrent, involuntary, and intrusive memories. Note: Children older than six may express this symptom in repetitive play.
- ii. Traumatic nightmares. Note: Children may have frightening dreams without content related to the trauma(s).
- iii. Dissociative reactions (e.g., flashbacks) which may occur on a continuum from brief episodes to complete loss of consciousness. Note: Children may reenact the event in play.
- iv. Intense or prolonged distress after exposure to traumatic reminders.
- v. Marked physiologic reactivity after exposure to trauma-related stimuli.
- The traumatic event is persistently re-experienced in the following way(s): (one required)
- Criterion C: avoidance
- Persistent effortful avoidance of distressing trauma-related stimuli after the event: (one required)
- i. Trauma-related thoughts or feelings.
- ii. Trauma-related external reminders (e.g., people, places, conversations, activities, objects, or situations).
- Persistent effortful avoidance of distressing trauma-related stimuli after the event: (one required)
- Criterion D: negative alterations in cognitions and mood
- Negative alterations in cognitions and mood that began or worsened after the traumatic event: (two required)
- i. Inability to recall key features of the traumatic event (usually dissociative amnesia; not due to head injury, alcohol, or drugs).
- ii. Persistent (and often distorted) negative beliefs and expectations about oneself or the world (e.g., "I am bad," "The world is completely dangerous").
- iii. Persistent distorted blame of self or others for causing the traumatic event or for resulting consequences.
- iv. Persistent negative trauma-related emotions (e.g., fear, horror, anger, guilt, or shame).
- v. Markedly diminished interest in (pre-traumatic) significant activities.
- vi. Feeling alienated from others (e.g., detachment or estrangement).
- vii. Constricted affect: persistent inability to experience positive emotions.
- Negative alterations in cognitions and mood that began or worsened after the traumatic event: (two required)
- Criterion E: alterations in arousal and reactivity
- Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic event: (two required)
- i. Irritable or aggressive behavior
- ii. Self-destructive or reckless behavior
- iii. Hypervigilance
- iv. Exaggerated startle response
- v. Problems in concentration
- vi. Sleep disturbance
- Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic event: (two required)
- Criterion F: duration
- Persistence of symptoms (in Criteria B, C, D, and E) for more than one month.
- Criterion G: functional significance
- Significant symptom-related distress or functional impairment (e.g., social, occupational).
- Criterion H: exclusion
- Disturbance is not due to medication, substance use, or other illness.
Furthermore, there are two specifications that must also be assessed; dissociative specification and delayed specification. For dissociative specification, in addition to meeting criteria for diagnosis an individual experiences high levels of either of the following in reaction to trauma-related stimuli:
- Depersonalization: the experience of being an outside observer of or detached from oneself
- Derealization: the experience of unreality, distance, or distortion
For delayed specification, full diagnostic criteria are not met until at least six months after the trauma(s) occurred, although onset of symptoms may occur immediately (American Psychiatric Association, 2013).
Traditional Treatments
There are a great number of traditional treatments available for PTSD patients with varying degrees of effectiveness, however, we will only examine the two most prominent categories and their most effective corresponding treatment: exposure therapy and pharmaceutics.
i. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a short-term, goal-oriented, talk exposure therapy treatment that takes a practical approach to problem solving. This therapy introduces patients to a set of principles that will last a lifetime and can be applied whenever they deem it appropriate. It can be thought of as a combination of psychotherapy and behavioral therapy and is considered advantageous in that it tends to be short in duration, on average taking between five to ten months for most emotional problems to be resolved or controlled (Martin, 2016). The psychotherapy emphasizes the importance of the personal meaning we place on things and how thinking patterns begin in childhood, while the behavioral therapy pays close attention to the relationship between our problems, behavior and thoughts (Friedman, Keane, Resick, & Ebooks Corporation, 2014). The goal of the CBT treatment is to change how a person thinks and feels by changing their pattern of thinking or behavior by focusing on the thoughts, images, beliefs, and attitudes behind a patient's difficulties. Although CBT is used to help treat a wide range of issues in a person’s life – including sleeping difficulties, relationship problems, substance abuse, anxiety, and depression – new research has shown CBT to be highly effective for PTSD patients (LeBlanc, Regehr, Jelley, & Barath, 2007).
ii. Pharmaceutics
As a therapist is not always available to be present with the patient, most forms of therapy are accompanied by a pharmaceutical treatment as well. The pharmaceutical drug Zoloft (Sertraline) is a selective serotonin re-uptake inhibitor and was introduced by Pfizer in 1991 as a suitable antidepressant. It was approved by the FDA in 1992 for commercial use and to date is the most effective pharmaceutical treatment available for PTSD patients with more than 50% of those suffering from long-term PTSD responding positively within just two weeks of treatment. It is administered orally via tablet or oral concentrate once per day with a dosage between 50 mg to 200 mg, depending on the patient’s requirements as prescribed by their psychiatrist, and cannot be taken in conjunction with a monoamine oxidase inhibitor (U.S. Food & Drug Administration, 1991). The duration of the treatment is at the discretion of the psychiatrist with respect to the prognosis of the patient’s symptoms.
Alternative Treatments and Technologies
In addition to traditional therapies, there are also currently a wide range of alternative treatments or technologies available for treatment. Again here we will examine the two most prominent alternatives relative to our proposed research: virtual reality and electroencephalography.
i. Virtual Reality (VR)
Virtual reality is a system that creates an artificial environment, which is experienced through sensory stimuli by using multi-projected environments, sometimes in combination with physical environments or props, to generate realistic images and sounds that stimulate the user's physical presence in a virtual world and enables the user's actions to partially determine what occurs within the environment (Fuchs, Moreau, & Guitton, 2011). Since 1995, researchers have been experimenting with using virtual reality exposure therapy (VRET) as a form of treatment for mental health disorders. Albert Rizzo from the University of Southern California’s Institute for Creative Technologies, with research funding from the Office of Naval Research, started validating a tool with other researchers nicknamed Virtual Iraq that they created using assets from the game Full Spectrum Warrior, which showed a normalization of over 70% in PTSD patients (Rizzo et al., 2008). VRET has now become the standard accepted technology-assisted treatment by the Anxiety and Depression Association of America, despite the Department of Veteran Affairs continuing to emphasize traditional exposure therapies as the recommended treatment. As a result, military research labs have subsequently set up numerous VRET labs for treating PTSD and other medical conditions. A meta-analysis of PTSD treatment done in 2012 further provided evidence that VRET can be as effective as traditional exposure therapies, if not more (Gonçalves, Pedrozo, Coutinho, Figueira, & Ventura, 2012). It can also be particularly effective for those resistant to traditional exposure treatments and is often used for war veterans, but has also been used with active-duty soldiers as well. It was also found that after only 6 sessions of VRET, post-treatment symptoms of PTSD were significantly reduced (Reger & Gahm, 2008).
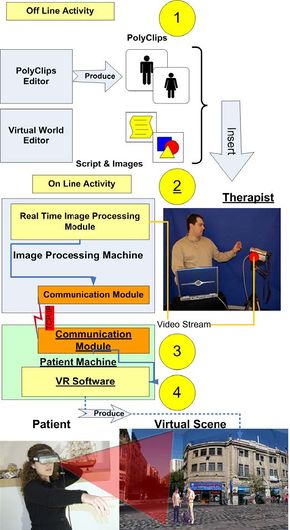
Unfortunately, current VR systems in use for therapy require that the patient become audio-visually isolated from real-life by having the patients use a head-mount display (HMD) and earphones. This means that during the patient’s immersion into the virtual world, they cannot make use of the support of their therapist. The latest advancement in the field of VRET has been the development of the ARGAMAN Software Suite which overcomes this barrier. The ARGAMAN system presented in Dayan's paper (2006) is composed of several subsystems and software structures that work together to create the VR environment offline. These subsystems comprise of 2 software editors: (i) polyclip editors that create animated actors, which are then inserted into the 3D environment of the virtual scenery; and (ii) virtual world editors that produce a Extensible Markup Language (XML) file, a program language paradigm that defines a set of rules for encoding documents in a format that is both human and machine readable, which will later be used by the software to describe the layout of the virtual world (Figure 3). With the help of these editors, the system is able to rapidly simulate the audio-visual environment where the patient’s trauma took place in 3D and generate realistic avatars that imitate people in that virtual environment. Consequently, this allows the patient to gradually understand and process the experience they had, visualize a recreation of their trauma while not being in any immediate danger, construct new memories of alternative scenarios, and face previously suppressed thoughts and emotions (Dayan, 2006). In addition, the system is unique in that it also provides the ability for the therapist to immerse themselves into the virtual world they have created for their patient (Figure 3.), enabling the therapist to be virtually present when their patient is re-experiencing their traumatic event and help them step-by-step through the experience. The level of exposure can be increased gradually over time in order to slowly accustom the patient to the stimuli. It is shown in another study that by receiving just 10 sessions of VRET resulted in significant reductions of PTSD symptoms of re-experience, avoidance, and emotional numbing individuals whom had experienced PTSD after a serious automobile accident (Beck, Palyo, Winer, Schwagler, & Ang, 2007).
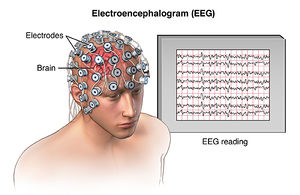
ii. Electroencephalography (EEG)
The electroencephalogram was invented in 1924 by the German psychiatrist, Hans Berger, and is a test that can detect brain wave abnormalities or neural electrical activity. It is a non-invasive brain-imaging technique that requires small electrodes contain metal discs with thin wires to be attached to the patient's scalp, which then detect small electrical charges that result from brain activity. The charges are amplified and appear as a graph on a computer (Figure 4.), which are then interpreted by the psychiatrist. This form of brain-imaging is advantageous because: it is much less expensive than other forms of brain imaging, such as functional magnetic resonance imagery (fMRI) or magnetoencephalography (MEO); is much easier to maintain and use; and is more tolerant to movement produced by the subjects. In a study by Lobo et al. (2015), it was found that there is a strong correlation between the type of neural activity recorded using an EEG and the severity of symptoms of patients suffering from PTSD. As well, it was also discovered that PTSD participants demonstrated a greater response to event related potentials (ERP) – the measured brain response in results from a specific sensory, motor, or cognitive event – in particular the P2 and P3 ERP's as well as alpha rhythms, all of which differed significantly from participants in the control group (Lobo et al., 2015). This information suggests that EEG's can indeed be used during PTSD therapies to monitor brain activity and responses to trauma stimuli presented during treatment.
Proposal, Research Question, and Hypothesis
Previous studies have found evidence that indicates exposure therapy is most effective when participants are subjected to trauma-provoking events similar to those they have personally experienced, but only up to a point where they do not enter a state of overwhelming fear or severe anxiety (Clark et al., 2009). A major disadvantage of current PTSD therapies is that aside from self-report tests taken either during or at the end of a treatment session, these treatments lack the ability of the therapist to actively monitor patient brain activity and response. Our proposed idea is a combined virtual reality electroencephalogram (VR-EEG) head-mount display (Figure 5.) that would target this drawback, thus enabling therapists to actively monitor brain activity to receive instant biofeedback and adjust patient exposure levels in accordance with their response to trauma stimuli presented in virtual reality.
What we are interested in researching is the effectiveness of the proposed VR-EEG treatment and whether it is:
- as effective as the current leading traditional form of therapy
- more effective than current leading traditional form of therapy
- as effective as standalone VR therapy
- more effective than standalone VR therapy
With respect to the above research questions, we hypothesize that:
- since virtual reality has already displayed significantly improved effectiveness relative to traditional exposure therapies, the addition of an EEG should not have a drastic effect and our proposed VR-EEG treatment will be more effective than a traditional CBT treatment done in conjunction with a Zoloft prescription
- because the VR-EEG treatment will allow a therapist to monitor their patient's brain activity and make appropriate adjustments during treatment that will reflect the patient's state-of-mind, it will be more effective than standalone VR treatment and will make the treatment become more personalized for each individual patient while ensuring maximal recovering with minimal consequences
Integration Disciplines
This multidisciplinary project will integrate 2 different fields within the realm of cognitive systems: computer science and psychology. The computer science discipline will cover the technological aspects of the research: the virtual reality system, head-mount displays, and the ARGAMAN software. The psychology discipline will cover the scientific aspects of the research: post-traumatic stress disorder and electroencephalography. The project will also touch on philosophy by examining consciousness during VR usage and the ethical concerns surround the design of this proposed VR-EEG treatment.
Methods
Sample Population & Experimental Groupings
For this experimental study, 200 participants will be randomly selected from a list of PTSD patients whom have been undergoing a combined cognitive behavioral therapy and Zoloft treatment (CBT-Z) at psychiatry clinics for a minimal period of 6 to 12 months. The specified sample size will ensure that our sample population will not only encompass different demographic areas but will also allow for a variety of different traumatic cases to be present within the sample population and is large enough to be statistically significant. As well, because patients who newly begin a CBT-Z treatment are subjective to drastic fluctuations in their state-of-mind as a result of drug-dosage correction and adaptation to cognitive behavioral therapy techniques, participants are selected whom have been already undergoing treatment for a minimal period of 6 to 12 months to help ensure that they have established some relative stability in their treatment progression. The participants will be divided into 5 treatments groups (Groups A – E), with Group A serving as the control group and each individual group consisting of 40 participants. The study will transpire over the course of one full year and will be divided into 3 stages, with each stage being 4 months in duration and each participant receiving 2 treatment sessions per week.
Since the participants that are randomly selected for the study are already receiving a combined CBT-Z treatment and each individual varies in how much they have progressed from their initial state and how far along in their treatment they currently are prior to beginning the study, Stage 1 of the experiment will consist of all participants in all groups to continue receiving their combined CBT-Z treatment for a duration of 4 months under supervision. This stage will allow researchers to establish a baseline for each participant and to evaluate their progression or regression throughout the study in accordance with this baseline. As Group A is the control group, it will consist of participants only receiving a CBT-Z treatment at all stages of the study. At Stage 2, Group B will be given a standalone VR treatment in conjunction with their CBT-Z treatment and Group C will be given the proposed VR-EEG treatment, while Group D and Group E will continue receiving only the CBT-Z treatment. At Stage 3, Group B and Group C will now revert back to receiving only a CBT-Z treatment , while Group D will now begin receiving VR treatment in conjunction with their CBT-Z treatment and Group E will be given the proposed VR-EEG treatment. All groups will be receiving a CBT-Z treatment at all stages, regardless of whether they receive a form of VR treatment or not. The treatment groups and stages are summarized in Figure 6.
Screenings and Treatment Evaluations
Prior to commencing the study, all participants will undergo a screening period during which researchers will evaluate each participant using two different interviews. For the first interview, participants will be describing the type of traumatic scenario they had experienced and detailing specific aspects of the scenario including scenery, the people involved, any objects involved, and sensory inputs they remember from the environment. Researchers will use this information to recreate an identical or near-identical environment in the virtual world that is specific to each participant’s experience. For the second interview, participants will be evaluated using the Clinician-Administered PTSD Scale (CAPS-5; Weathers et al., 2017). This 30-item structured interview follows a 5-point scaling system – with 0 being absent and 4 being extreme – and is used to assess the 20 PTSD symptoms outlined by the DSM-5 and includes questions that target the following aspects:
- current symptoms
- severity of symptoms
- onset and duration of symptoms
- impact of symptoms on social and occupational functioning
- overall response validity
A CAPS-5 total symptom severity score is calculated by summing severity scores for the 20 DSM-5 PTSD symptoms (Weathers et al., 2017). This initial screening is important in allowing researchers to establish a baseline for each participant for future referencing during the study.
Over the course of the treatment, researchers will further continually assess participants at 2 frequencies: (i) self-report tests using the Impact of Event Scale – Revised (IES-R; Weiss & Marmar, 1997) at the end of each treatment session and (ii) interview using CAPS at the end of every month. The IES-R is a 22-item self-report test that follows a 5-point scaling system – with 0 being “not at all” and 4 being “extremely" – and assesses the subjective distresses caused by traumatic events. This test will only be used to determine participant progression or regression as it cannot be used for diagnosis (Weiss & Marmar, 1997).
Once the study is completed, participants will undergo a final exit interview that will include one final CAPS assessment and an experiment debriefing.
Variables
In this study, the independent variable is the form of treatment we provide to each participant at the respective stage over time and the dependent variable is the amount of symptom reduction they display (measured using CAPS and IES-R scoring, then inversely converted to a percentage) relative to the form of treatment they received.
Anticipated Results
It is important to note here that anticipated results explained in this section are purely hypothetical and any numerical values used are arbitrary and for representation of general trends only. They are by no means representations of actual data. During the study, researchers assessed participants at 2 frequencies using 2 scales: an Impact of Event Scale – Revised (IES-R) after every treatment session and a Clinician-Administered PTSD Scale (CAPS) at the end of every month. The scores participants receive on the CAPS and IES-R are inversely proportional to the percentage of symptom reduction meaning that a lower score on either scale is an indication of a higher percentage of symptom reduction. Therefore we would expect participants who received standalone VR treatment in conjunction with the CBT-Z treatment to have lower scores on both scales in comparison to the control group that received only CBT-Z treatment. Furthermore, because the VR-EEG treatment would be the most effective, we would expect participants who received the proposed VR-EEG treatment in conjunction with the CBT-Z treatment to have even lower scores than both the participants who received the standalone VR treatment in conjunction with CBT-Z and and those in the control group who received only CBT-Z treatment.
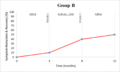
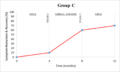
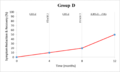
During Stage 1, all groups receive the same CBT-Z treatment, therefore, it is expected that all participants will averagely display the same amount of symptom reduction. We will designate here a hypothetical reduction of symptoms by 10% for all participants. Because Group A is serving as the control group and will receive only CBT-Z treatment at each stage, we can assume Group A participants will have another 10% reduction during Stage 2 and another 10% reduction during Stage 3 for a net reduction of 30% once the study is completed (Figure 7.1). At Stage 2, Group B and Group C participants will continue to receive CBT-Z treatment, however, here Group B will receive an additional standalone VR treatment while Group C will receive the proposed VR-EEG treatment. Because VR has already demonstrated to be more effective than CBT-Z, we can expect to see both groups receiving a form of VR treatment to show increased symptom reduction in comparison to control Group A. However, because the VR-EEG treatment would be more effective than standalone VR, the percentage of symptom reduction after receiving the VR-EEG should hypothetically be higher than the standalone VR (Figure 7.2 and Figure 7.3 respectively). Group B will be designated a hypothetical reduction of symptoms by 30% in Stage 2 while Group C is designated 50%. Group D and Group E will both continue receiving CBT-Z treatment only in this stage so we can assume that participants of both groups will have a hypothetical 10% reduction in symptoms. At Stage 3, Group B and Group C will both revert back to only receiving CBT-Z treatment, therefore we can expect to see the percentage of symptom reduction for both groups to fall back to 10%. Now Group D and Group E participants will continue to receive CBT-Z treatment, however, here Group D will receive an additional standalone VR treatment while Group E will receive the proposed VR-EEG treatment. We expect that percentage of symptom reductions for Group D and Group E in Stage 3 to be identical to those of Group B and Group C in Stage 2, therefore, Group D will be designated a hypothetical 30% symptom reduction in Stage 3 while Group E is designated 50% (Figure 7.4 and 7.5 respectively).
Based on this hypothetical data, we can expect participants in Group B and Group D whom received standalone VR treatment to display a greater net reduction of symptoms (50%) than those in control Group A (30%), while participants in Group C and Group E whom received the proposed VR-EEG treatment to display an even greater net reduction of symptoms (70%) than those in Group A, Group B, and Group D. The following 5 graphs represent anticipated results for each treatment group with their corresponding hypothetical percentage of symptom reduction:
- widths=300px
Possible Sources of Error
Although researchers will take all appropriate measures to ensure that the data they collect will be as accurate and precise as possible, there are inevitably certain confounding variables that they cannot determine or control. The following are possible confounding variables that may have an effect on collected data:
- Age: the age of the participants may have an effect on how they respond to the virtual reality.
- Degree of Embodiment: depending on how realistic and engaging the virtual environment appears to the participant, it could cause varied results for each participants and would affect how the exposure treat works.
- Diet: changes in diet may have an impact on the effectiveness of Zoloft. This may be caused by certain food molecules to act as antagonists to Zoloft receptors or perhaps cause an increase or decrease in endogenous neurotransmitters that bind to Zoloft receptors.
- Lifestyle: participants make changes to their lifestyle that may have an impact on their reactivity to treatment and progression. These may include changes to their daily routine (i.e. exercise, meditation, etc.), fluctuation of stress hormones, increased or decreased social interactions, or changed sleeping patterns.
- Rating Effect: participants may have biased responses in terms of how they feel about using VR for treatment and how they view their progression through treatment.
- Standard Deviation: although not a confounding variable, if the standard deviation between participants is very large, it would indicate a fundamental flaw in the method hence render the data unreliable.
- Tolerance: participants may have already developed tolerance for Zoloft when they are randomly selected to take part in the study or may possibly develop tolerance over the course of the study.
Discussions
Reasoning for Proposed Idea
According to the U.S. Department of Veteran Affairs (2016), approximately 6 out of 10 males and 5 out of 10 females experience at least one form of trauma during their lifetime. Of those, approximately 8% go on to develop fully-diagnosed PTSD. With a population of about 340 million people, that equates to roughly 27 million American citizens who suffer from PTSD. And although there has been much more attention being focused on this mental health disorder over the years, there is a lack of research that compares the different types of treatment available for patients. The best form of traditional exposure therapy currently available is cognitive behavioral therapy (CBT) which is supplemented with a Zoloft prescription and the best technology-assisted treatment available is virtual reality. All forms of therapy, however, lack the ability to actively monitor patient's brain activity and response to stimuli during treatment and instead resort to using self-report measures either during or once the treatment has completed. The proposed HMD not only has the potential to illustrate factors that cannot be assessed using self-reports measures, but it also removes the aspect of delayed response (whereby patients undergo treatment and only once completed do they reflect on their state-of-mind and provide a self-report) that significantly alters self-report answers given by patients.
Reasoning for Method
The method used ensures that the proposed VR-EEG treatment is being compared with the most effective treatments available. The selected sample size of n=200 ensures that the sample population is both large enough for any changes that occur to be statistically significant and diverse enough to encompass different demographic areas. As well, it will provide participants who have experienced different forms of trauma and allow the proposed treatment to be used for different PTSD cases and scenarios. Group A serves as the control group and allows researcher to compare the standalone VR treatment and the proposed VR-EEG treatment to a consistent trend line. Each group has its specified form of treatment both added and removed at different stages over the course of the study so it can be compared to the baseline and determined whether the specific form of treatment does indeed display an improvement in symptom reduction or not.
Virtual Reality Design Ethics
As we are applying technology in a human relation, it is interesting to investigate how the design of a VR application determines or influences the actions the users perform in its virtual environment and the ways these users experience these actions and learn from them. VR is therefore a form of humanized technology, as it takes into account the biological sensory and emotional aspects of our being. Modeling the world in VR is a human practice in which we engage with the world in our process of understanding it (Jones, 2000). Usually, the relation between virtual reality worlds and the real world range from similar to completely different. On one end of the spectrum, some VR models have been designed to authentically portray existing structures or events. However, VR worlds usually found in video games often display fantasy worlds with no intended correspondence with any objects or properties in the real world, and may even break physical laws (Bray, 1999). For example, in relation to exposure therapy in PTSD, rooting from military occurrences, a VR simulation of military combat can be programmed to look realistic to different degrees. Choices must be made in this design, concerning the level of detail and realism by which objects or features included in the simulation are represented. In a VR representation of combat for example, wounds may be represented as faint dots or may be represented in full graphic detail. According to research conducted by Bray (1999), there are two types of representational failures or shortcomings in VR:
- Misrepresentation: in which some aspects of the simulation are clearly mistaken according to accepted standards of accuracy. For example, there may be selective misrepresentations or idealized representations of objects, including icons or symbols, for pragmatic purposes. In a simulation of surgery, organs and tissues may be rendered in unrealistic colors to facilitate recognition. In a simulation of combat, it may be convenient to remove targets that have been killed or destroyed from the simulation because they no longer serve a purpose to be present.
- Biased representation: in which the values or interests of some stakeholders of the simulation are insufficiently accounted for. For example, the use of stereotypes in the representation of people, things, and events may not be factually incorrect, in that they might exist in reality as they are represented, but may rest on stereotypes that are not representative of reality at large. In particular, the representation of individuals and their behaviors and cultural artifacts may be based on ethnic or gender stereotypes.
Both these representational failures can induce false or biased beliefs in users and can ultimately have undesirable consequences. Representational biases can make VR less useful or agreeable to users whose values or interests are omitted in the application. One might argue that VR simulation is vastly value laden, and it is problematic if the users of VR hold certain values or have certain interests that may be compromised or may fail to be promoted in the VR.
Implications of Consciousness
Virtual reality aims to provide virtual stimuli that is equivalent to our surroundings in the real world. If this is obtained, then the brain activity should respond to VR stimuli, just as it does to real world stimuli, which we are able to measure using EEG. The physiological experience is the same: electrical signals are passed up your optic nerve and between different areas of your brain to produce an output. But this is not the complete experience, and you might argue that there is also a subjective aspect. For instance, when you look at a painting, you are directly experiencing the colors and structures, but at the same time, you may be feeling some emotions or subjective thoughts forming in response to the painting. Chalmers (1995) believed that together these experiences make up what we know as consciousness - the subjective inner life of the mind. But what forms this subjective response? He referred to this as "the hard problem” and the question is how physical processes in the brain give rise to subjective experience. This puzzle involves the inner aspect of thought and perception: the way things feel for the subject. For instance, when we see, we experience visual sensations; when we hear, we experience auditory input. But it is still subjective as to whether we prefer the color red or blue, or if we enjoy rock music over classical. It is very difficult to explain what causes this. Now, if we are exposed to the same stimuli in VR, does the brain know that it’s not real, it is conscious? If we produced the same brain activity to the stimuli in VR as to the real world, then what really distinguishes VR from the real world? And if there is no difference, then why would it be wrong to want to live in VR instead of the real world? These problems are very hard to unlock, but perhaps the data from the VR-EEG study will provide a further understanding to how the brain reacts to VR stimuli and this may serve as a step in the direction to understand how we form subjective experiences and from there gain more knowledge about consciousness.
Pros and Cons
The growing technological advances in virtual reality have opened many new research possibilities and applications in behavioral neuroscience. As virtual reality technology matures, even greater potential extents for the controlled study and manipulation of the human organism and mind (Tar & Warren, 2002). There are many pros regarding VR. It can be used as a learning tool, as for example flight simulator or similar. In therapy VR can also be used in exposure therapy for people with phobias, and for example the fear of rattlesnakes or tropical animals are much easier to access in a VR environment, rather than actually providing a real thing for the patient to confront. In the future, almost every stimulus associated with phobias could be presented in VR. VR can also replicate places that no longer exist, and it is further possible to recreate an event or experience. However, this might be subject to misrepresentation and biases, and one might argue that this is not ethically sound. VR can easily be used to promote stereotypes, or even propaganda, and be used as a tool to affect the end user in a certain direction. Right now, VR is expanding vastly and is getting incorporated into many professional fields. One might argue that we should take a much more critical stand towards VR, and consider carefully how the design affects the user, and how thing should be presented.
Conclusion
This project aims to use real-time biological feedback in order to create a more effective and personalized treatment for a devastating, life-changing disorder. Those suffering from PTSD need the best treatment possible in order to regain normal daily life and recover from the trauma they experienced. Implications from this research could affect treatment of other mental health disorders, helping professionals use biofeedback and computerized systems to help people in the best way possible.
Bibliography
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). Washington, D.C: American Psychiatric Publishing.
Beck, J. G., Palyo, S. A., Winer, E. H., Schwagler, B. E., & Ang, E. J. (2007). Virtual reality exposure therapy for PTSD symptoms after a road accident: An uncontrolled case series. Behavior Therapy, 38(1), 39-48. doi:10.1016/j.beth.2006.04.001
Bray, P. (1999). The ethics of representation and action in virtual reality. Ethics and Information Technology, 1(1), 5-14. doi:10.1023/A:1010069907461
Chalmers, D. J. (1995). The puzzle of the conscious experience. Scientific American, 273(6), 80-86.
Clark, C. R., Galletly, C. A., Ash, D. J., Moores, K. A., Penrose, R. A., McFarlane, A. C. (2009). Evidence-based medicine evaluation of electrophysiological studies of anxiety disorders. Clinical EEG and Neuroscience, 40(2), 84-112. doi:10.1177/155005940904000208
Dayan, E. (2006). ARGAMAN: Rapid deployment virtual reality system for PTSD rehabilitation. Paper presented at the 34-38. doi:10.1109/ITRE.2006.381528
Friedman, M. J., Keane, T. M., Resick, P. A., & Ebooks Corporation. (2014). Handbook of PTSD: Science and Practice (2nd ed.). New York: The Guildford Press.
Fuchs, P., Moreau, G., & Guitton, P. (2011). Virtual reality: Concepts and Technologies. Boca Raton, FL: CRC Press.
Gonçalves, R., Pedrozo, A. L., Coutinho, E. S. F., Figueira, I., & Ventura, P. (2012). Efficacy of virtual reality exposure therapy in the treatment of PTSD: A systematic review. PloS One, 7(12), e48469. doi:10.1371/journal.pone.0048469
Jones, S. (2000). Towards a philosophy of virtual reality: Issues implicit in “Consciousness Reframed". Leonardo, 33(2), 125-132. doi:10.1162/002409400552388
LeBlanc, V. R., Regehr, C., Jelley, R. B., & Barath, I. (2007). Does posttraumatic stress disorder (PTSD) affect performance? The Journal of Nervous and Mental Disease, 195(8), 701-704. doi:10.1097/NMD.0b013e31811f4481
Lobo, I., Portugal, L. C., Figueria, I. Volchan, E., David, I., Pereira, M. G., & Oliveira, L. (2015). EEG correlates of the severity of posttraumatic stress symptoms: A systematic review of the dimensional PTSD literature. Journal of affective disorders, 183, 210-220. doi:10.1016/j.jad.2015.05.015
Martin, B. (2016). In-Depth: Cognitive Behavioral Therapy. Psych Central. Retrieved from https://psychcentral.com/lib/in-depth-cognitive-behavioral-therapy/
National Center for PTSD. (2015). Women, Trauma, and PTSD. Retrieved from https://www.ptsd.va.gov/public/PTSD-overview/women/women-trauma-and-ptsd.asp
National Center for PTSD. (2017). Understanding PTSD and PTSD Treatments. Retrieved from https://www.ptsd.va.gov/public/understanding_ptsd/booklet.pdf
Reger, G. M., & Gahm, G. A. (2008). Virtual reality exposure for active duty soldiers. Journal of Clinical Psychology, 64(8) 940-946. doi: 10.1002/jclp.20512.
Rizzo, A. A., Graap, K., Perlman, K., McLay, R. N., Rothbaum, B. O., Reger, G., . . . Pair, J. (2008). Virtual Iraq: Initial results from a VR exposure therapy application for combat- related PTSD. Studies in Health Technology and Informatics, 132, 420-425.
Tarr, M., & Warren, W. (2002). Virtual reality in behavioral neuroscience and beyond. Nature Neuroscience, 5(11s), 1089-1092. doi:10.1038/nn948
U.S. Department of Veterans Affairs. (2016). How Common is PTSD? Retrieved from https://www.ptsd.va.gov/public/PTSD-overview/basics/how-common-is-ptsd.asp
U.S. Food & Drug Administration. (1991). Zoloft (sertraline hydrochloride). Retrieved from https://www.fda.gov/Drugs/DrugSafety/ucm085729.htm
Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., & ... Marx, B. P. (2017). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and Initial Psychometric Evaluation in Military Veterans. Psychological Assessment, doi:10.1037/pas0000486
Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event Scale—Revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing Psychological Trauma and PTSD. New York: Guilford Press.