Course:MEDG550/Student Activities/Criduchatsyndrome
Cri-du-chat syndrome
Cri-du-chat syndrome (CdCS) is a rare genetic condition that a person can be born with. People who have CdCS often have a cat-like cry when they are born, grow slower than people at the same age, have learning difficulties that impact their daily lives, and may not hit their milestones like walking or talking at the expected times. [1]. These common features are due to a change in one of the person's chromosomes, which will be described in the section Genetics and Inheritance. The syndrome and its cause were first described by Lejeune et al. in 1963 [2]
Clinical Features
General Features[1]
- Intellectual disability: learning difficulties that can impact their daily lives
- Delayed development: delay in hitting their childhood milestones
- Small when growing during pregnancy which continues after birth
- Cat-like cry at birth
- Feeding difficulties
Craniofacial abnormalities: affecting the skull and face [1]
- Round face
- Small head
- Widely spaced and downward slanting eyes
- Down-turned corners of the mouth
- Irregularly shaped ears
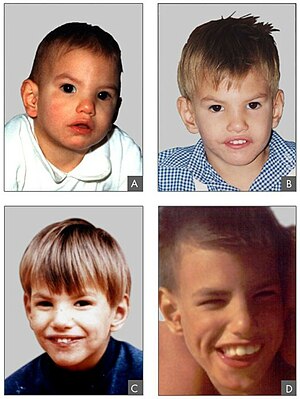
It is important to note that the cat-like cry disappears during the first few years of life, although the timbre of voice may remain abnormal[3]. Timbre is a term used to describe the quality of tone of voice. As a child with CdCS matures, their face becomes long and slender. Their eyes are no longer wide-spaced and their small head becomes more evident[4]. At birth and as the child moves into toddlerhood, they often are "floppy" because they do not have the same amount of muscle mass or tone as toddlers without CdCS. As they age, the floppy characteristics are replaced with muscle stiffness due to too much muscle tone.
Other features include heart problems including ventricular and atrial septal defects[1]. Sometimes, children will be born with a single line of the palm of their hand instead of the expected two or more. Occasionally, an individual with CdCS may have additional problems, including kidney problems (ex. horseshoe kidney) or problems with brain function (ex. cerebral atrophy). Other infrequent features include scoliosis, ear tags, cleft lip and palate and nearsightedness[1].
Generally children with CdCS have a gentle and affectionate personality, although some behaviour problems may occur. Predominant behavioural problems include hyperactivity, loss of attention, uneasiness, aggressive and self-injured behaviour[3]
Genetics and Inheritance
Our bodies are made of billions of cells. In each of our cells, we have a recipe book that tells our cells what to make for every part of our body. These recipe books are packaged up into structures called chromosomes, which are like chapters in the book. In our bodies we have 46 chromosomes in all of our cells. All 46 chromosomes add new information and are important to make what the body needs to work as expected. Each of these chromosomes is made of 2 sections which scientists call "arms". The smaller section of a chromosome is called the p arm, and the longer section of the chromosome is called the q arm. Sometimes, pieces of chromosomes can move around when they are in the cell and pieces can be lost or rearranged to join other chromosomes.
This recipe book is made up of genes, which tell the body to make proteins, that help the body grow and develop when it is supposed to. Proteins are the building blocks to the different tissues and organs that make up our bodies. Genes can also tell cells when to become different tissues, because we need certain tissues at different times during our lifespan. We inherit our genes from our parents, half of them from your mom and the other half from your dad. People get different combinations of their genes to make you, you. Everyone has changes in their genes, which makes all humans unique.
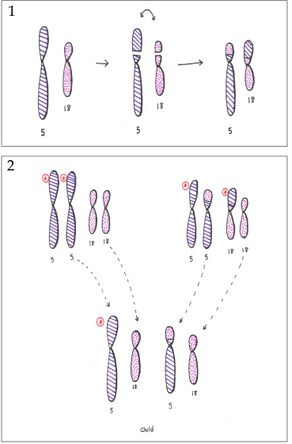
In CdCS, one of the arms of chromosome 5 has some missing genes. When there is genes missing, scientists and members of the medical team call this a deletion. The deletion in Cri-du-chat syndrome is on the p arm (the small arm) of chromosome 5. Deletions may vary greatly between individuals with CdCS. Two regions have been found to be deleted in all individuals with CdCS[1][5]. 15.2 and 15.3 refer to a specific area on the p arm of the chromosome.
- 5p15.2
- 5p15.3
The region at 5p15.2 is associated with the main clinical features of CdCS. The 5p15.3 region is specifically associated with the cat-like cry. Although larger deletions are usually associated with a more severe phenotype, it is impossible to determine or predict what the condition will look like for individuals that have it.
It is estimated that Cri-du-chat syndrome occurs in about 1/20,000 to 1/50,000 births, regardless of ethnic background. This makes it one of the more common chromosomal deletion syndromes [4].
Most cases of CdCS are de novo, [3] meaning the deletion happened by a random event during the formation of the egg or sperm, or during early development of the embryo. This means that usually there is no family history of the condition.
In approximately 10% of cases, the parents of a child with CdCS have a balanced rearrangement[1]. This means that while they have all the appropriate amount of genetic material (nothing missing or extra), the rearrangement means their offspring have a higher chance of having missing or extra genetic material. In this case, there is a higher chance of having another child with CdCS or another genetic condition and/or a higher chance of frequent miscarriages. The chances of these outcomes depends on several factors, such as the type of rearrangement, the chromosomes involved and the size of the pieces arranged.
Diagnosis and Management
Diagnosis for Cri-du-chat syndrome may be done based on clinical features only. Genetic confirmation may be done looking at the chromosomes (particularly the p arm of chromosome 5) via karyotype or specifically only looking at the critical region of CdCS using Fluorescence in situ hybridization (FISH). A microarray may also be able to detect smaller imbalances in the CdCS region. Other investigations, such as an MRI or a speech and language assessment, may be ordered to better understand the severity of the diagnosis and appropriate interventions.
As CdCS is a genetic condition, there is no cure. Individuals with CdCS benefit greatly from early interventions, including physiotherapy, occupational therapy and speech therapy. Other health professionals who may be helpful include a dietician, a psychologist, an audiologist and an ophthalmologist. Surgeons and other specialties may become involved depending on individual needs. With the support of their family and healthcare professionals, individuals with CdCS are able to live full and meaningful lives.
Given that developmental and behavioral characteristics are commonly associated with CdCS, it may be beneficial to parents to prepare for their children acquiring a special-needs education program. In countries such as Australia, Canada, New Zealand, and the USA, there are opportunities for children diagnosed with CdCS to receive education assistance through an individualized education plan (IEP). In these countries, IEPs form the basis for which children with developmental and physical disabilities can acquire a rigorous and meaningful education. According to current best-practice principles, When an IEP is able to become established early using a collaborative approach between parents and education professionals, the educational goals of the child can be successfully identified and established. In this scenario, priorities are focused on the actual procedures that will be implemented in an attempt to achieve those educational goals for the child [6].
Genetic Counselling Considerations
For those with a family history or those living with Cri-du-Chat syndrome, genetic counselling can provide several benefits. A genetic counsellor can explain the cause, the symptoms of the disorder, as well as facilitate genetic testing. They can also provide support for parents and families during their emotional journey. A genetic counsellor may be able to provide more details on:
Genetic testing: if a couple has a child affected with Cri-du-chat syndrome, it is recommended that both parents are tested for a balanced rearrangement. Although the syndrome is primarily de novo, individuals with a balanced rearrangement involving 5p are at an increased risk of having another child with Cri-du-chat syndrome. If a parent is identified to be a carrier of such a rearrangement, his/her family members are also at risk of having the same rearrangement and should be offered genetic testing.
Prenatal diagnosis: invasive testing is available to families where one parent is a known carrier of balanced structural arrangement. Cells may be obtained by Chorionic villus sampling or amniocentesis and analyzed using cytogenetic methods.
Recurrence risk: the risk of having another child with CdCS
- for a carrier parent of a structural rearrangement: there is an increased risk of having another child with a genetic condition, although the exact risk would depend on several considerations, such as the type of rearrangement and the size of the region(s) involved
- for individuals with Cri-du-chat syndrome: the recurrence risk is estimated to be 50%
- for parents with no cytogenetic abnormalities identified: the recurrence risk is less than 1%
Support Groups
Having CdCS or supporting a family member with CdCS may be extremely challenging. Support groups are beneficial, providing further information on the condition and tips for management. They are also an excellent source for support, allowing families to interact locally and globally.
Australia
Cri du chat support group of Australia
Canada
Canadian Organization for Rare Disorders
United Kingdom
Cri du chat syndrome support group
United States
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Mainardi, P.C. (2006). Cri du Chat syndrome. Orphanet Journal of Rare Diseases, 1, 33-39.
- ↑ Lejeune, J., Lafourcade, J., Berger, R., Vialatte, J., Boeswillwald, M., Seringe, P., Turpin, R. (1963). Trois cas de délétion partielle du bras court d'un chromosome 5. Comptes Rendus de l’Académie des Sciences (D), 257, 3098-3102.
- ↑ 3.0 3.1 3.2 Rodriguez-Caballero, A., Torres-Lagares, D., Rodriguez-Perez, A., Serrera-Figallo, M.-A. Hernandez-Guisado, J.-M., Machuca-Portillo, G. (2010). Cri du chat syndrome: a critical review. Medicina Oral, Patologia Oral, Cirugia Bucal, 1, c473-478.
- ↑ 4.0 4.1 Niebuhr E. (1978). The cri du chat syndrome. Epidemiology, cytogenetics and clinical features. Human Genetics, 44, 227–275.
- ↑ Overhauser, J., Huang, X., Gersh, M., Wilson, W., McMahon, J., Bengtsson, U., … Wasmuth, J.J. (1994). Molecular and phenotypic mapping of the short arm of chromosome 5: sublocalization of the critical region for the cri-du-chat syndrome. Human Molecular Genetics, 3, 247–252.
- ↑ Pituch KA, Green VA, Didden R, Whittle L, O’Reilly MF, Lancioni GE, Sigafoos J. Educational Priorities for Children with Cri-Du-Chat Syndrome. J Dev Phys Disabil. Feb 2010; 22(1): 65–81